Review Article - (2024) Volume 15, Issue 11
Abstract
Improving patient outcomes depends critically on the early identification of breast cancer. Artificial Intelligence (AI) has the potential to completely transform Breast Cancer (BC) screening by enabling detection up to five years before a clinical diagnosis. This paper examines this possibility and explores the most recent developments in AI algorithms, particularly in relation to medical imaging, such as mammography.
We investigate how AI can identify precancerous alterations that are often invisible to the human eye by analyzing minute patterns in breast tissue. Additionally, we discuss the challenges and opportunities associated with developing and evaluating AI models for early detection, including issues of model interpretability, data quality and ethical considerations.
The ultimate goal of this analysis is to demonstrate how AI can significantly reduce BC mortality by facilitating much earlier detection.
Keywords
Artificial Intelligence, Breast Cancer, Personalized medicine, Digital mammography, Breast tissue
Introduction
For many years, intelligent computer systems have played a significant role in society. Research and development in AI have garnered interest across various sectors, including the economy, government, industry, technology, healthcare and security and defence (Plan S, 2016). The use of AI is currently evolving in many disciplines due to the convergence of innovative AI approaches, immense computational power and the widespread increase in digital data gathering and storage, particularly in science and health.
In the field of cancer care, AI systems are being created, investigated and tested for disease detection, prognostication and as support tools for clinical decision-making. Current research on BC represents an international effort to develop sophisticated Machine Learning (ML) algorithms for analyzing screening mammograms, which could enhance BC screening by reducing false positives (Houssami N, et al., 2017).
AI applications in BC diagnostics extend beyond imaging to include the interpretation of pathology results (Figure 1). For instance, AI has assisted in identifying metastatic BC in whole slide images during sentinel lymph node biopsies. This work focuses on understanding how contemporary AI systems can improve screening procedures for the early identification of BC (Wang D, et al., 2016).

Figure 1: Representation of AI in the health care system.
BC has become the most commonly diagnosed disease, surpassing lung cancer, with approximately three million cases and 700,000 fatalities recorded in 2020 (Sung H, et al.,2021). The annual incidence of BC has been increasing since the mid-2000s; however, there has been a significant decline in the mortality rate associated with the disease (Figure 2).
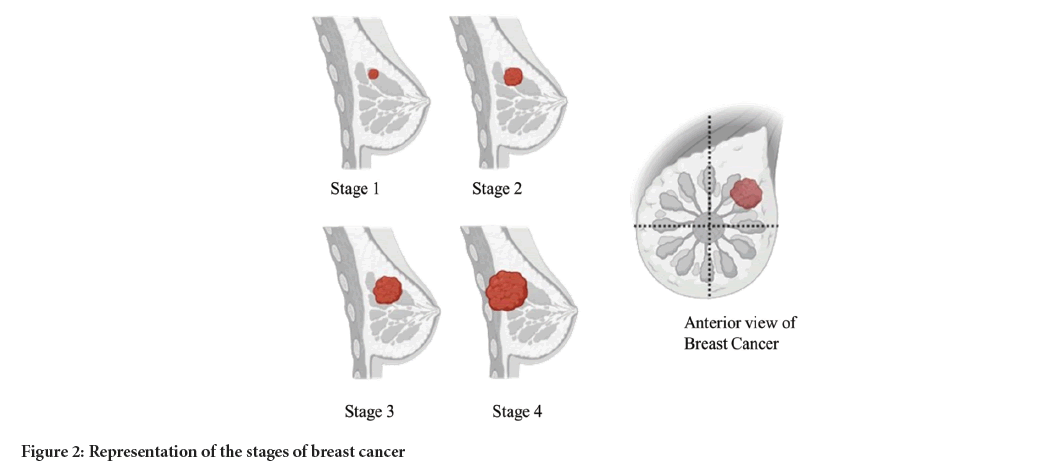
Figure 2: Representation of the stages of breast cancer.
Mortality trends differ by ethnicity. Non-Hispanic White (NHW) individuals have higher rates of BC compared to Non-Hispanic Black (NHB) individuals; however, NHW individuals have experienced a greater decline in mortality rates than their NHB counterparts. As a result, NHB individuals face higher mortality rates despite having lower incidence rates than NHW individuals (Martini R, et al., 2022).
Many screening programs are primarily based on age, which is the most frequently researched risk factor for breast cancer. However, the disease can also develop due to various other factors (Pike MC, et al., 1983). Important risk factors include high Body Mass Index (BMI), a history of hyperplastic or neoplastic breast disease and a family history of breast cancer.
Additionally, long-term estrogen exposure whether from early menstruation or late menopause is another significant risk factor (Jakes RW, et al., 2000).
Literature Review
We conducted a literature search from 2010 to 2018 to review advances in AI methods for BC detection. This review focused on studies assessing AI approaches in screening, specifically those that included quantitative performance data compared to established standards.
Eligible studies evaluated AI in BC screening among women, without restriction to those with a history of cancer or biopsy. We excluded studies that involved simulated lesions, those lacking performance data and studies with fewer than 100 subjects or 200 images. Additionally, commentary articles, editorials, reviews and conference abstracts were also excluded from our analysis.
The impact of AI on healthcare diagnostics
AI is transforming healthcare, particularly in diagnostic processes. Physicians utilizing AI to interpret images and diagnose patients more accurately can save lives (Stoitsis J, et al., 2006).
The two primary subfields of AI are ML and Deep Learning (DL). ML enables computers to discover patterns and insights by learning from data and making predictions without explicit programming. In contrast, DL goes a step further by learning directly from unprocessed data, eliminating the need for human-defined features. This capability makes DL especially effective for deciphering complex data patterns and facilitates more automated and sophisticated learning processes.
AI holds immense promise for medical imaging. It can assist radiologists in analyzing results, optimizing imaging systems and automatically identifying lesions in various organs. AI-driven Computer-Aided Detection (CADe) systems enhance diagnosis and prognosis by providing second opinions.
Furthermore, AI improves image post-processing tasks such as segmentation and registration (Choy G, et al., 2018).
Current methods of BC detection
International approaches to BC screening vary significantly. In the United States and similar countries, women seeking screening may either self-refer or be referred by their doctors to screening institutions. These institutions differ in their screening methodologies and image interpretation practices.
Conversely, many European nations have government-run screening programs that utilize standardized tools and processes. Women enrolled in these programs are periodically invited for screenings and those who exhibit any abnormalities are referred to hospitals for further assessment (Figure 3).
Figure 3: Representation of current methods used in the detection of breast cancer.
Digital Mammography (DM): BC screening practices vary globally. In countries like the United States, screening is often institution-based, with women either self-referring or being referred by their doctors. The methods of screening and image interpretation can differ significantly between institutions.
In contrast, many European countries have government-run screening programs that utilize standardized procedures and equipment. Women participating in these programs receive periodic invitations for screening and any suspicious findings typically result in referrals to hospitals for further evaluation (Thomassin NI, et al., 2019).
DM offers several advantages over traditional film mammography, one of which is a more efficient workflow. While DM is largely similar to film mammography for the general population, it has demonstrated better performance in certain patient groups. Additionally, digital technology enables the development of sophisticated image processing tools and advanced imaging techniques, such as tomosynthesis and dedicated breast Computed Tomography (CT) (Skaane P, 2009).
Despite the advancements in imaging technology, both film-based and DM are limited by their two-dimensional representation of a three-dimensional breast. This limitation presents a significant challenge known as tissue superposition, where overlapping structures can obscure underlying abnormalities. To mitigate this issue, standard mammography protocols involve taking two orthogonal views of each breast: The Mediolateral Oblique (MLO) and Cranio-Caudal (CC) projections. Radiologists carefully compare these images to identify potential lesions, considering factors such as lesion shape, density, margins and calcifications.
However, the limitations of 2D imaging frequently lead to missed cancers, particularly in women with dense breast tissue, where malignant lesions can be obscured by overlapping glandular tissue.
Digital Breast Tomosynthesis (DBT): Over the last 20 years, the development and clinical acceptance of DBT have been driven by the inherent limitations of standard 2D mammography. DBT addresses the issue of overlapping tissue artifacts associated with traditional mammography by capturing multiple images of the breast from various angles, providing a pseudo-3D perspective. As a result, DBT has demonstrated increased cancer detection rates and typically lower recall rates compared to DM, particularly in scenarios where the initial DM recall rate was high (Ciatto S, et al., 2013).
However, interpreting DBT images is more time-consuming due to the greater number of image slices compared to standard mammograms. This presents a significant challenge for the widespread implementation of DBT in screening programs. To overcome this obstacle, automated techniques are essential.
AI can play an important role by accelerating navigation through the image stack and assisting in lesion detection, thereby significantly reducing the workload for radiologists.
Moreover, AI can help standardize interpretation, which may enhance the consistency of DBT's impact on cancer detection rates across different studies. By improving efficiency and accuracy in image interpretation, AI has the potential to further optimize the benefits of DBT in BC screening.
Conventional techniques used in detecting BC: The transition from film to DM has led to the development of two main categories of computer-assisted techniques for detecting breast cancer: CADe and Computer-Aided Diagnosis (CADx).
CADe focuses on identifying potential abnormalities, such as masses or clusters of micro calcifications. Traditional CADe systems operate in three steps: First, the image is pre-processed to enhance suspicious features; second, the system identifies potential areas of interest; and third, these regions are evaluated to determine the likelihood of a true abnormality. Regions that exceed a certain threshold are then flagged for radiologist review (Ganesan K, et al., 2012).
In contrast, CADx systems assess the likelihood that a detected lesion is benign or malignant. While CADx and the final phase of CADe are comparable, CADx does not rely on a simple threshold for evaluation.
Both conventional CADe and CADx systems depend on pre-programmed features that instruct computers on what to search for based on specific traits associated with concerning lesions. This approach differs significantly from contemporary AI-based techniques. Researchers have developed algorithms that analyze breast images in a manner that mimics human interpretation processes, thereby enhancing CADe performance. One method involves comparing similar characteristics between the same and different breasts to improve detection accuracy (van ES, et al., 2007).
Limitations and challenges of these conventional
The assessment of the efficacy of conventional BC detection algorithms is complicated by the fact that various algorithms currently utilize different testing data and methodologies. Additionally, there is a lack of independent studies that evaluate their effectiveness (Topol EJ, 2019).
One significant challenge is the scarcity of high-quality, labelled and representative data, particularly regarding the distribution of pathologies, demographics and breast density. Most available research datasets are limited in scope and often originate from a single institution or a specific mammography machine vendor, which can lead to overfitting of algorithms.
To facilitate independent testing with fresh datasets and to minimize bias from recurring situations, the data used for training, validating and testing AI systems should be made publicly accessible.
Moreover, since the ground truth significantly influences algorithm performance, it is important that this data is reliable.
Potential biases must also be considered before implementing AI in clinical practice. One such bias is known as the anchoring effect, which occurs when an image contains indicators suggesting potential cancer. This can lead viewers to over-rely on these indicators, skewing their judgment and potentially affecting diagnostic accuracy.
Addressing these limitations and challenges is essential for improving the reliability and effectiveness of BC detection technologies (Becker AS, et al., 2017).
AI algorithms and technology
Recent studies have compared the performance of DL, Convolutional Neural Networks (CNNs) to conventional methods such as CADe and CADx in the early stages of BC diagnosis through mammography. For example, Bruno MA, et al., 2015 conducted a study to identify masses in DBT and found that DL improved sensitivity for suspicious lesions from 83.2%-89.3% and for malignant lesions from 85.2%-93.0%.
In another early study, Becker AS, et al., 2017 tested the effectiveness of DL against radiologists instead of using traditional CADe. They utilized a commercial deep learning-based image analysis method that was not authorized for medical use and was originally designed for industrial applications. Two distinct datasets were employed: One contained an equal mixture of 50% malignant and 50% control instances, while the other, which more closely mirrored real screening settings, comprised approximately 10% malignant and 90% control cases. The findings indicated that DL algorithms, even those intended for non-medical imagery, could be trained to identify BC in digital mammography, despite the second dataset having substantially higher cancer prevalence than actual screenings.
In the high prevalence group, two of the three readers significantly outperformed the algorithm; however, in the lower prevalence set, the algorithm's performance was comparable to that of the radiologists (Kooi T, et al., 2017).
Benefits of early detection
Early identification of illnesses, particularly cancer, offers several advantages that significantly enhance patient outcomes. One of the primary benefits is that early diagnosis typically leads to easier treatment and management, thereby increasing the likelihood of survival.
With early identification, patients often require less aggressive therapies, which can reduce both physical and psychological stress. Additionally, early detection can help avoid the costly treatments associated with advanced stages of illness, ultimately lowering healthcare expenses.
Moreover, prompt treatment can halt the progression of the disease, improving the quality of life for affected individuals and their families. By identifying health problems before they worsen, early diagnosis supports better long-term health and well being. These benefits underscore the critical importance of early detection in improving patient outcomes and optimizing healthcare resources (Shaikh K, et al., 2021).
Future prospects
Future advancements in imaging technology, including more sophisticated Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) scanners as well as the development of liquid biopsies, are set to revolutionize early illness identification and treatment. These innovations will provide less intrusive screening options and yield higher-quality images.
AI will play an important role in the medical field by rapidly and accurately analyzing vast amounts of data, identifying trends and abnormalities and customizing treatment regimens based on a patient's genetic makeup and medical history. When integrated with wearable medical technology, AI-powered solutions will enhance diagnostic precision and facilitate real-time patient monitoring.
This combination of AI and wearable devices will enable early illness diagnosis, leading to prompt treatments and improved patient outcomes. As these technologies continue to evolve, they hold the promise of transforming healthcare delivery and enhancing the overall quality of care for patients.
Current state of art AI algorithms for DM and DBT
CNNs are currently the foundation of the most advanced AI algorithms for identifying and categorizing lesions in mammography and DBT. Several companies have developed commercial AI applications that have received approval from the Food and Drug Administration (FDA) or are currently in the final stages of review.
To assess the efficacy of a commercial AI system for DM, Rodriguez Ruiz and colleagues collected nine datasets from locations in the United States and Europe. These datasets included Probability of Malignancy (POM) ratings and DM images from studies comparing DM with other imaging modalities.
The study involved breast screening performed by radiologists, culminating in a final dataset comprising 2,652 examinations from four different suppliers, which included 653 instances of cancer. A total of 28,296 separate interpretations of the images were produced from the assessments of 101 radiologists (Rodriguez RA, et al., 2019). At the case level, the performance of the AI system was statistically no worse than the average performance of these radiologists.
Notably, the AI outperformed 61% of the individual radiologists when comparing its performance to that of each reader.
The robustness of this extensive study is attributed to the diversity of the data and the large number of cases and readers involved. The research included images from systems manufactured by four distinct vendors and interpretations from radiologists across seven different countries, encompassing varied screening practices. The Receiver Operating Characteristic (ROC) curves demonstrated that the AI's performance was consistently comparable to that of the radiologists, regardless of whether prior tests were considered in the evaluation.
This body of research underscores the potential for AI algorithms to enhance BC detection capabilities in both DM and DBT, paving the way for improved diagnostic accuracy and patient outcomes in BC screening (Kim EK, et al., 2018).
Graphical abstract
This study, however, did not entirely resolve all issues and does not adequately predict how AI would perform in actual BC screenings compared to human radiologists. Some of the datasets were unilateral, others excluded previous images and all were enhanced and evaluated in a laboratory environment. Radiologists often rely on the ability to compare recent images with older ones, but AI systems are not yet capable of doing this. Despite these drawbacks, the performance of radiologists was not significantly impacted in comparison to the AI, even when previous images were available.
Determining any bias in the study's results may be challenging due to factors such as laboratory settings and non-screening illness prevalence that may have influenced the findings. Thus, while this comprehensive analysis provided valuable insights regarding the current level of AI assessment in DM, further research is necessary ideally involving large scale datasets to evaluate radiologist performance in real screening scenarios.
Very large training datasets are needed for whole image classification techniques that are not trained with annotated images.
Furthermore, these approaches require additional procedures to indicate to users where concerning discoveries are located. For example, Kim EK, et al., 2018 trained, validated and tested a DL using a CNN that could classify images as malignant or not. The model produced heat maps indicating the areas that contributed most to the final classification decision, using a dataset of over 4,000 cancer cases and nearly 25,000 normal cases, all without pixel level annotations (Figure 4).

Figure 4: Representation of graphical abstract for AI detection of breast cancer.
Conclusion
Computers are becoming increasingly adept at identifying BC in mammograms. While they show great promise, additional research is still needed to determine their effectiveness. Scientists have utilized images from various locations and medical professionals to test AI. Although the AI performed reasonably well, it remains unclear whether it can detect cancer as accurately as human doctors can. This uncertainty arises because the computer was trained on unique images that were not representative of typical examinations.
Furthermore, physicians often use AI to detect changes in patient records by comparing recent images to older ones.
To truly understand how AI functions, it is essential to test it on a large number of standard images. If successful in doing so and continuing to enhance the AI's capabilities, it could assist doctors in finding cancer earlier and ultimately save lives.
References
- Plan S. The national artificial intelligence research and development strategic plan. National Science and technology council, networking and information technology research and development subcommittee. 2016.
- Houssami N, Lee CI, Buist DS, Tao D. Artificial intelligence for breast cancer screening: Opportunity or hype?. The Breast. 2017; 36: 31-33.
[Crossref] [Google Scholar] [PubMed]
- Wang D, Khosla A, Gargeya R, Irshad H, Beck AH. Deep learning for identifying metastatic breast cancer. 2016.
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71(3): 209-249.
[Crossref] [Google Scholar] [PubMed]
- Martini R, Newman L, Davis M. Breast cancer disparities in outcomes; unmasking biological determinants associated with racial and genetic diversity. Clin Exp Metastasis. 2022; 39(1): 7-14.
[Crossref] [Google Scholar] [PubMed]
- Pike MC, Krailo MD, Henderson BE, Casagrande JT, Hoel DG. Hormonal risk factors, breast tissue age and the age-incidence of breast cancer. Nature. 1983; 303(5920): 767-770.
[Crossref] [Google Scholar] [PubMed]
- Jakes RW, Duffy SW, Gao F. Mammographic parenchymal patterns and risk of breast cancer at and after a prevalence screen in singaporean women. Int J Epidemiol. 2000; 29(1): 11-19.
[Crossref] [Google Scholar] [PubMed]
- Stoitsis J, Valavanis I, Mougiakakou SG, Golemati S, Nikita A, Nikita KS. Computer aided diagnosis based on medical image processing and artificial intelligence methods. Nucl Instrum Methods Phys Res. 2006; 569(2): 591-595.
- Choy G, Khalilzadeh O, Michalski M, Samir AE, Pianykh OS, Geis JR, et al. Current applications and future impact of machine learning in radiology. Radiology. 2018; 288(2): 318-328.
[Crossref] [Google Scholar] [PubMed]
- Thomassin NI, Balleyguier C, Ceugnart L, Heid P, Lenczner G, Maire A, et al. Artificial intelligence and breast screening: French Radiology Community position paper. Diagn Interv Imaging. 2019; 100(10): 553-566.
[Crossref] [Google Scholar] [PubMed]
- Skaane P. Studies comparing screen-film mammography and full-field digital mammography in breast cancer screening: Updated review. Acta Radiol. 2009; 50(1): 3-14.
[Crossref] [Google Scholar] [PubMed]
- Ciatto S, Houssami N, Bernardi D, Caumo F, Pellegrini M, Brunelli S, et al. Integration of 3D digital mammography with tomosynthesis for population breast-cancer screening (STORM): A prospective comparison study. Lancet Oncol. 2013; 14(7): 583-589.
[Crossref] [Google Scholar] [PubMed]
- Ganesan K, Acharya UR, Chua CK, Min LC, Abraham KT, Kwan Hoong Ng. Computer-aided breast cancer detection using mammograms: A review. IEEE Rev Biomed Eng. 2012; 6: 77-98.
[Crossref] [Google Scholar] [PubMed]
- van Engeland S, Karssemeijer N. Combining two mammographic projections in a computer aided mass detection method. Med Phys. 2007; 34(3): 898-905.
[Crossref] [Google Scholar] [PubMed]
- Topol EJ. High-performance medicine: The convergence of human and artificial intelligence. Nat Med. 2019; 25(1): 44-56.
[Crossref] [Google Scholar] [PubMed]
- Becker AS, Marcon M, Ghafoor S, Wurnig MC, Frauenfelder T, Boss A. Deep learning in mammography: Diagnostic accuracy of a multipurpose image analysis software in the detection of breast cancer. Invest Radiol. 2017; 52(7): 434-440.
[Crossref] [Google Scholar] [PubMed]
- Bruno MA, Walker EA, Abujudeh HH. Understanding and confronting our mistakes: The epidemiology of error in radiology and strategies for error reduction. Radiographics. 2015; 35(6): 1668-1676.
[Crossref] [Google Scholar] [PubMed]
- Kooi T, Litjens G, van GB, Gubern MA, Sánchez CI, Mann R, et al. Large scale deep learning for computer aided detection of mammographic lesions. Med Image Anal. 2017; 35: 303-312.
[Crossref] [Google Scholar] [PubMed]
- Shaikh K, Krishnan S, Thanki RM. Artificial intelligence in breast cancer early detection and diagnosis. Cham: Springer. 2021.
- Rodriguez RA, Lang K, Gubern MA, Broeders M, Gennaro G, Clauser P, et al. Stand-alone artificial intelligence for breast cancer detection in mammography: Comparison with 101 radiologists. J Natl Cancer Inst. 2019; 111(9): 916-922.
[Crossref] [Google Scholar] [PubMed]
- Kim EK, Kim HE, Han K, Kang BJ, Sohn YM, Woo OH, et al. Applying data-driven imaging biomarker in mammography for breast cancer screening: Preliminary study. Sci Rep. 2018; 8(1): 2762.
[Crossref] [Google Scholar] [PubMed]
Author Info
Prasurjya Saikia1*, Durgaprasad Kemisetti2, Ananga Mohan Das1, Charlisar Teron2 and Diptimonta Neog32Department of Pharmaceutical Sciences, Assam down town University, Gandhi Nagar, Guwahati, Assam, India
3Department of Physics, North Eastern Regional Institute of Science and Technology, Nirjuli, Arunachal Pradesh, India
Citation: Saikia P: Artificial Intelligence in Early Detection: Identifying Breast Cancer Before Clinical Diagnosis
Received: 01-Nov-2024 Accepted: 21-Nov-2024 Published: 30-Nov-2024, DOI: 10.31858/0975-8453.15.11.345-349
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






