Case Report - (2022) Volume 13, Issue 11
Boerhaave’s Syndrome: A Case Report
Mahmoud Saqr1, Ahmed Almasloot2*, Mahmoud Eltawagny1 and Osama Hawana1Abstract
Background: Spontaneous oesophageal rupture is a rare presentation which requires a high level of clinical suspicion.
Case presentation: A 39-y-old patient presented with atypical symptoms of severe abdominal pain, constipation, and vomiting.
Results: Abdominal pain resolved after initial treatment, thought to have acute abdominal pathology, initial chest X-ray and abdominal X-ray were normal studies with no identified acute pathologies.
Discussion: The patient was kept under observation till deterioration happened; a Computed Tomography scan (CT scan) was done for suspected intra-abdominal sepsis, and then images showed a ruptured oesophagus. Eventually, the patient was admitted for urgent surgical intervention.
Conclusion: This case report describes a rare Emergency Department (ED) presentation which requires a high index of suspicion, early diagnosis, and urgent management.
Keywords
Boerhaave syndrome, Oesophageal perforation, Rupture oesophagus, Spontaneous oesophageal rupture
Abbreviations
CT: Computed Tomography; ED: Emergency Department; SBP: Systolic Blood Pressure; RR: Respiratory Rate; NPO: Nil per Oral; IV: Intravenous; CBC: Complete Blood Count; URTI: Upper Respiratory Tract Infection; AUD: Alcohol Use Disorder; CTICU: Cardiothoracic Intensive Care Unit; OGD: Oesophago-Gastro-Duodenoscopy; GEJ: Gastro-Esophageal Junction; CXR: Chest X-Ray
Introduction
Boerhaave’s syndrome is a rare but serious condition that is characterized by oesophageal non-traumatic rupture, it usually happens after forceful vomiting. If not diagnosed and treated early, it can be fatal. Challenge is the variation in clinical pictures and presentations (Kopelman Y, et al., 2018). It requires urgent intervention in most of the cases (Tiago C, et al., 2022). Epidemiological data regarding oesophageal perforation is sparse. In a national study in Iceland, the incidence was reported as 3.1 per million populations (Vidarsdottir H, et al., 2010). A systematic review reported that spontaneous oesophageal perforation incidence among the other causes of rupture is 38% (Sdralis EI, et al., 2017). A case of postoperative oesophageal rupture was reported (Atallah FN, et al., 2004). Around 70% of the oesophageal rupture is thoracic (Sancheti MS and Fernandez FG, 2015; Shaker H, et al., 2010). Clinical presentation usually depends on the site, size, and onset of perforation, according to Medscape: Patients with cervical oesophagus perforation may present with neck or upper chest pain. Patients with middle or lower oesophagus perforation may present with interscapular or epigastric discomfort. Findings of pleural effusion are common. If present, subcutaneous emphysema is particularly helpful in confirming the diagnosis. Subcutaneous emphysema is seen in 28%-66% of patients at initial presentation. More typically, subcutaneous emphysema is found later. Other classic findings include tachypnoea and abdominal rigidity.
Tachycardia, diaphoresis, fever, and hypotension are common, particularly as the illness progresses. However, these findings are non-specific. The mortality rate is about 13% (Sdralis EI, et al., 2017). Different diagnostic modalities are being used; CT confirmed the diagnosis (38.7%), X-ray (36.6%) and endoscopy (37.4%) (Sdralis EI, et al., 2017). Using CT scans with/without contrast media has a false negative rate of 10% (Shaker H, et al., 2010; Lázár G, et al., 2011). A rapid diagnosis with chest drains after diagnosing a left-sided pleural effusion/pneumothorax is indicative when the chest tube drains bile or food particles (Suzuki M, et al., 2012). Early management, involvement of senior experienced physician and early diagnosis has been shown to have a good impact on decreasing mortality (Zuleta GMA, et al., 2014). Treatment is usually surgical, depending on the severity of perforation, and some reports described recovery also after conservative management (de Schipper JP, et al., 2009). There is no clear data about the long-term survival rates after Boerhaave’s syndrome, some studies revealed three years survival of 90% with surgical treatment (de Schipper JP, et al., 2009).
Case Presentation
A 39-year-old patient presents to the emergency department in Hamad General Hospital in Qatar (a large tertiary hospital), the patient complained of severe abdominal pain and two episodes of forceful vomiting that had started 4 hours before he presented to the ED. The patient described the pain as severe generalized (all quadrants), colicky with no radiation to any area, he had constipation for 2 days, and no active vomiting on presentation. The patient had a history of chronic alcohol intake, last alcohol consumption wince one week (as per the patient himself). Examination revealed tenderness, and rigidity in all abdominal quadrants, and chest examination was normal. Vital signs were normal, blood pressure (Systolic BP-150), pulse 105/min, RR 20/min with normal temperature.
Treatment
After initial analgesia, the patient showed improvement and started to localize the pain to the
Epigastrium and periumbilical area. Given the history of alcohol consumption and normal chest and abdomen X-rays, the patient was investigated as a case of possible pancreatitis and was kept NPO (Nil per Oral). After 4 hours of observation, the patient was pain-free, still in constipation and had no vomiting. On further reassessment, the patient was not in severe pain, still constipating but had a normal bowel sound, and a rectal exam showed stool matter. Enema was given and patiently passed stool. The patient was kept for observation, IV antibiotics were commenced because he was febrile, and WBCs came higher in repeat CBC. He then gave a history of URTI cough and expectoration.
Results
Investigation
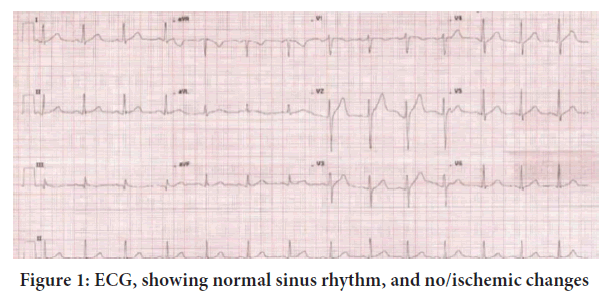
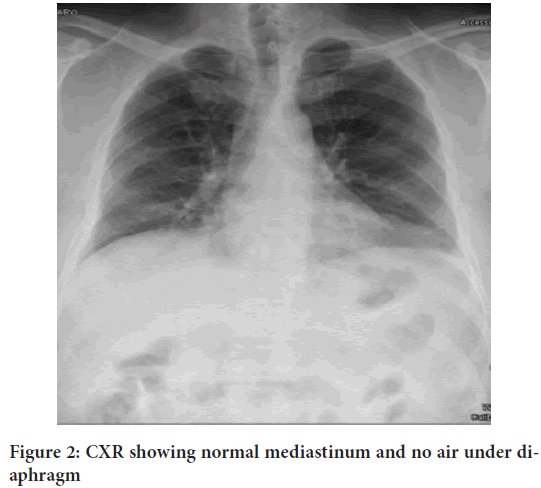
To rule out the acute cardiac event, an ECG, (Figure 1) was done, and it showed no acute ischemic signs. Immediate chest X-ray (Figure 2) and abdominal X-ray were obtained to rule out acute abdominal viscus perforation and intestinal obstruction, and both showed no air under diaphragm, normal mediastinum, and no air-fluid level in the abdomen.
| Haematology | Date and time | Unit measurement and reference range | |||
|---|---|---|---|---|---|
| 15/7/17 06:39 |
15/7/17 14:45 |
15/7/17 18:37 |
16/7/17 04:19 |
||
| WBC (White blood cells) | 18.2 | 24.4 | 25.1 | 24 | 4.5-11 × 1000/mm3 |
| RBC (Red blood cells) | 5.8 | 5.8 | 5.3 | 5.5 | 4.5-5.9 × 106/mm3 |
| Platelet | 155 | 153 | 151 | 150 | 150-450 × 1000/mm3 |
| MPV (mean platelet volume) | 11.1 | 10.8 | 11.3 | 11.3 | 8.9-11.8 fL |
| Neutrophils | 15.3 | 21.8 | 22.6 | 20.7 | 2%-7.5% |
Note: Normal RBCs, WBC count is building up with the neutrophils raising through the course of observation
Table 1: CBC showing leucocytosis and neutrophilia
Figure 1: ECG, showing normal sinus rhythm, and no/ischemic changes
Figure 2: CXR showing normal mediastinum and no air under diaphragm
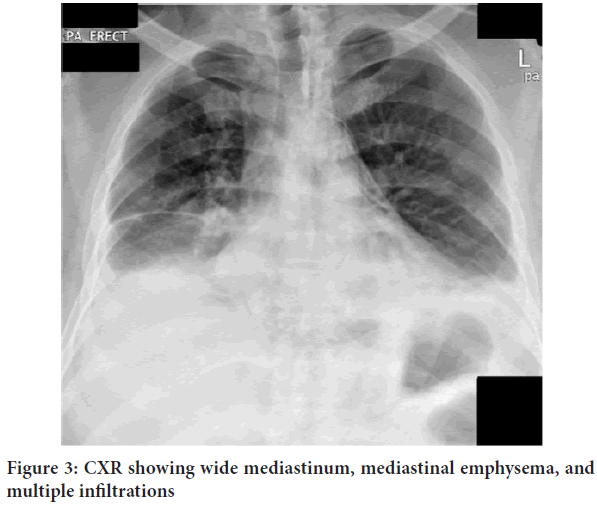
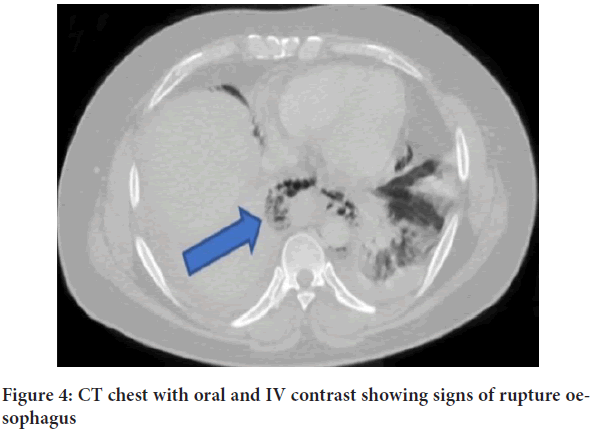
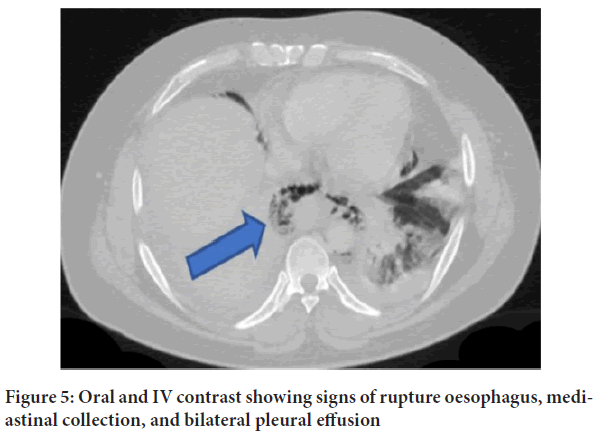
Blood investigations were done, CBC (Table 1) (Complete Blood Count) showed leucocytosis with neutrophilia and high normal Hb which implied dehydration, normal pancreatic enzymes, normal liver function tests (Table 2) normal renal functions, and mild hypokalaemia (Table 3). Ultrasound abdomen was done, and it was normal. After 24 hours in the observation unit, the patient started to develop chest pain, high-grade fever, and tachycardia. Antibiotics were changed to sepsis protocol and an immediate chest X-ray (Figure 3) was ordered. X-ray showed wide mediastinum with mediastinal emphysema, suspected AUD, and multiple infiltrations. Immediate CT chest with contrast oral and IV was ordered to investigate oesophageal rupture and it was positive for features suggesting oesophageal rupture with the mediastinal collection and pleural effusion (Figures 4 and 5).
| Liver function test | Date and time | Unit measurement and reference range | ||
|---|---|---|---|---|
| 15/7/17 06:39 |
15/7/17 21:05 |
16/7/17 04:19 |
||
| Albumin | - | 37 | 35 | 35-50 g/L |
| ALK Phos (Alkaline phosphatase) | - | 71 | - | 60-306 U/L |
| ALT (Alanine Transaminase) | - | 19 | - | Up to 42 U/L |
| AST (Aspartate aminotransferase) | - | Sample haemolyzed | - | Up to 37 U/L |
| Amy-p (Amylase) | 12 | - | - | 25-125 IU/L |
| Lipase | 17 | - | - | 10-140 IU/L |
| Glucose | 4.9 | - | - | 4-5.9 mmol/L |
| CRP (C Reactive Protein) | 46 | 172 | - | <10 mg/L |
| Lactic acid | - | - | 2.8 | 0.5-2.2 mmol/L |
Note: Normal levels of liver functions, lipase and amylase ruled out the acute pancreatitis and cholecystitis which raised more suspicion about the cause of symptoms
Table 2: Normal liver function results, normal amylase and elevated CRP
| Laboratory view | Date and time | Unit measurement and reference range |
|---|---|---|
| 15/7/17 06:39 |
||
| Na (sodium) | 135 | 135-145 mEql/L |
| K (potassium) | 3.3 | 3.6-5.2 mmol/L |
| Creatinine | 73 | 61.9-114.9 µmol/L |
| Lactic acid | 2.1 | 0.5-2.2 mmol/L |
| Troponin | <10 | <10 ng/mL |
Note: Normal serum electrolytes initially, normal creatinine level wasn’t pointing towards organ failure, also normal range of troponin with the initial ECG were not in favour towards acute cardiac event
Table 3: Mild hypokalaemia and normal troponin
Figure 3: CXR showing wide mediastinum, mediastinal emphysema, and multiple infiltrations
Figure 4: CT chest with oral and IV contrast showing signs of rupture
Figure 5: Oral and IV contrast showing signs of rupture oesophagus, mediastinal collection, and bilateral pleural effusion
surgery consultation was done, and a barium swallow was done which confirmed the diagnosis of intrathoracic oesophageal rupture. The patient was shifted to CTICU (Cardiothoracic Intensive Care Unit) where urgent endoscopy was done in the theatre. After admission, OGD was done and revealed oesophageal perforation at about 33 cm from the incisors, and the GEJ was at 40 cm at the oesophageal opening of the diaphragm. Treated with stenting which showed migration then it was replaced. The stent was removed after 6 weeks. The patient resumed feeding and was discharged home after 2 months of admission. The patient had his first follow-up in the clinic, and he was doing well eating all solid food with no sequel.
Discussion
In this case, we did not detail the surgical management as we focused on the emergency department course of the boerhaave’s syndrome and the challenges that encounter any clinician in the diagnosis. This case was very close to being named atypical presentation because of some points that ambiguated the diagnosis-
• The patient presented to ED with abdominal pain only, colicky in nature generalized, and he did not link the pain to vomiting. The pain was never in the chest, shoulders or back. Given the fact that the perforation was intrathoracic, however, the low site of perforation, only 7 cm above the diaphragm made the site of pain in the abdomen.
• Chest X-ray was taken 5 hours after symptoms and yet showed no changes at all. In our perspective, this could be explained by the containment of the perforation after the initial release of contents. And we favour that this increases the emphasis on low sensitivity for such tests to rule out the condition.
• The patient became pain-free after analgesia, his main complaint lately was fever, but because of inflammatory markers and initial presentation, he was not discharged.
• The concomitant occurrence of URTI and fever, which happened 3 days before presentation, hindered further investigating of the septic focus for such infection.
Conclusion
What we conclude from this case is that a high index of suspicion should be made for the diagnosis of spontaneous oesophageal perforations. Despite the fact being rare, Boerhaave’s disease should be on the list of possible diagnoses, especially if risk factors like alcoholism and a history of vomiting exist. Also, the diagnostic process should be guided by a clinical picture, but it should not only be bound to it. The presence of findings like leucocytosis and high inflammatory markers should widen the range of differential diagnoses and push to further diagnostic modalities, like early CT abdomen, even if pain improved in the case that definitive diagnosis is not already obtained.
Authors’ Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by Mahmoud Saqr, Ahmed Almasloot, Osama Hawana and Mahmoud Eltawagny. The first draft of the manuscript was written by Mahmoud Saqr and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethical Approval
The ethical approval is Exempt from the Medical Research Center at Hamad Medical Corporation, Doha, Qatar and Prince Sultan Military Hospital, Taif, Saudi Arabia. We certify that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
A sentence confirming that written informed consent was obtained from all participants or, if participants are under 16, from a parent and/or legal guardian.
Author Info
Mahmoud Saqr1, Ahmed Almasloot2*, Mahmoud Eltawagny1 and Osama Hawana12Department of Emergency Medicine, Prince Sultan Military Hospital, Taif, Saudi Arabia
Citation: Saqr M: Boerhaaveâ??s Syndrome: A Case Report
Received: 20-Oct-2022 Accepted: 03-Nov-2022 Published: 10-Nov-2022, DOI: 10.31858/0975-8453.13.11.768-772
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3