Review Article - (2023) Volume 14, Issue 5
Causative Factors, Diagnostic Testing and Management of Infertility
Chaudhari Hiral Shankarbhai1*, Dhiren L Chaudhari1 and Jalpa A Soni2Abstract
Infertility is a disease of the male or female reproductive system defined by the failure to achieve a pregnancy after 12 months or more of regular unprotected sexual intercourse. Infertility is classified as primary and secondary infertility. Primary infertility is inability to have pregnancy and secondary is inability to have a pregnancy after previously successful conception. There are certain factors such as male factors, female factors, unidentified factors and other factors which are responsible for the cause of infertility. Moreover, there are some diagnostic tests available for testing both male and female infertility through which the actual cause of the infertility can be known. To deal with this disease various treatments are available such as pharmacological and surgical treatments. Also, there are some prevention strategies that can be explained to avoid the chances of infertility.
Keywords
Infertility, Pregnancy, Reproductive system, Pharmacological treatment, Surgical treatment
Introduction
The World Health Organization (WHO) has described infertility as a “disorder of the reproductive system” resulting in a disability. Infertility is a disorder of both male and woman reproductive systems described via the failure to clinically being pregnant after three hundred and sixty-five days or everyday unprotected intercourse. Infertility occurs due to male elements, woman elements, and a mixture of male and woman factors or unexplained factors. People affected by this have higher costs of depression, anxiety, suicide, divorces, and intimate accomplice violence. Environmental and life-style elements consisting of smoking, excessive alcohol intake, obesity and exposure to environmental pollution have been related to decrease fertility in both male and female. It has an effect on the couple’s psychological, financial, scientific, and social wellness (WHO, 2020). It is a disease of the male or female reproductive system defined by the failure to achieve a pregnancy after 12 months or more of regular unprotected intercourse.
Literature Review
Epidemiology
Worldwide infertility has turn out to be an international health problem that’s affecting millions of people at their reproductive age. Infertility in girls is ranked the 5th highest critical international disability. On September 2020, WHO records estimates suggest that about 48 million couples and 186 million individuals have infertility problem globally (Mascarenhas MN, et al ., 2012). On August 2016, World Health Organization estimate that overall prevalence of primary infertility in India turned into 3.9% to 16.8%. In India, the prevalence of infertility varies from state to state and it also varies from tribes and caste. Prevalence of infertility in Indian states was 3.7% in Uttar Pradesh, Himachal Pradesh and Maharashtra, 5% in Andhra Pradesh, and 15% in Kashmir. In 2019, NCBI estimated that Male factors infertility contributes 30%-40% of infertility in couples and 40% of all causes of infertility can be completely due to female factors (Rastogi A, 2016). The burden of the sickness worldwide is excessive. It is envisioned that 34 million women, predominantly from developing international locations, are infertile.
Male infertility: Etiology
• Lifestyle factors (Weight problems, smoking, tablets and anabolic steroids).
• Azoospermia and oligozoospermia.
• Genetic abnormalities.
• Immunological sicknesses (Autoimmune disorders and antisperm antibodies).
• Systemic sickness (Diabetes, renal and liver insufficiency and cancers).
• Exogenous factors (Medicinal drugs, pollution and irradiation).
• Semen problem, vascular and Testosterone (T) issues.
• Endocrine disturbances.
Pathophysiology
The primary elements that are influencing the analysis of infertility are: Period of infertility; primary or secondary infertility; semen issues; age and fertility status of the woman partner, urogenital abnormalities, coital frequency and timing, in addition to this erectile disorder (NDP, 2019). Previous surgical operations, childhood illnesses and undescended testis results in male infertility. Medical history such as diabetes mellitus and upper respiratory disease, chronic medication, history of Sexually Transmitted Infections (STI’s), smoking, alcohol, recreational tablets use, and anabolic steroid use and exposure to gonad toxins (e.g: Chemotherapy and radiation remedy) also are accountable for inflicting infertility.
Diagnosis
General physical examination: General physical examination has to be achieved wherein the secondary sex characteristics, body habitus, hair distribution, breast improvement, penile abnormalities, the testis quantity, and the presence of a varicocele should be taken into consideration. In instances of azoospermia, palpation for the presence of the vas deference must be examined.
Semen analysis: Semen evaluation must be finished and interpreted. In case of a regular semen analysis, there is no requirement for semen evaluation and andrological tests. In case of bizarre semen analysis, a repeat semen analysis should be achieved, and similarly andrological tests need to be accomplished through health practitioner. The results of semen analysis must be compared with the World Health Organization reference values. If end result is observed to be odd, then confirmatory test should be conducted after three months, so that time for the cycle of spermatozoa formation may be finished. If gross azoospermia or excessive oligozoospermia has been detected the test should be repeated as quickly as possible (Table 1).
| Parameters | Lower reference limit |
|---|---|
| Semen volume (ml) | 1.5(1.4-1.7) |
| Total sperm number (106 per ejaculate) | 39(33-46) |
| Sperm concentration (106 per ml) | 15(12-16) |
| Total motility (PR+NP, %) | 40(38-42) |
| Progressive motility (PR, %) | 32(31-34) |
| Vitality (live spermatozoa, %) | 58(55-63) |
| Sperm morphology (normal forms, %) | 4(3.0-4.0) |
| Other consensus threshold values | |
| pH | ≥ 7.2 |
| Peroxidase positive leukocytes (10° per mi) | <1.0 |
| Mixed erythrocyte-spermatozoa Antiglobulin Reaction (MAR) test (motile spermatozoa with bound particles, %) | <50 |
| Immunobead test (motile spermatozoa with bound beads, %) | <50 |
| Seminal zinc (umol/rejaculate) | ≥ 2.4 |
| Seminal fructose (umol/ejaculate) | ≥ 13 |
| Seminal neutral glycosidase (mU/ejaculate) | ≥ 20 |
Note: Lower reference limits (5th centiles and their 95% confidence intervals) for semen characteristics; NP: Non-Progressive motility
Table 1: WHO reference values for semen characteristics
Special investigations
• Endocrine evaluation-Initially, assessment of hormones that include measurement of serum Follicle Stimulating Hormone (FSH), Luteinizing Hormone (LH), prolactin, and overall Testosterone (T) concentrations in instances of azoospermia or excessive oligospermia. If the preliminary checks found to be abnormal, then huge evaluation has to be taken into consideration.
• Ultrasonography-Scrotal ultrasound assists as an addition to bodily examination and to exclude testicular tumors. Varicoceles that aren’t palpable clinically and best identified with ultrasound are not clinically applicable. Urologist ought to do this evaluation.
• Post-ejaculatory urinalysis-A post-ejaculatory urinalysis is accomplished having an ejaculate quantity less than 1 ml. The urine is alkalized and post-masturbation is finished, then urine is centrifuged and tested underneath high magnification. The presence of sperm within the postejaculatory urinalysis shows retrograde ejaculation.
• Tests for anti-sperm antibodies are very controversial and recurring checking out isn’t always encouraged.
• Testis biopsy or aspiration is taken into consideration in guys with azoospermia. Here spermatozoa are present; which might be frozen for the use in assisted duplicate.
Investigation for infections
Testing for infection like Human Immunodeficiency Virus (HIV) and Hepatitis, Rubella IgG and Chlamydia should be finished:
• People who undergo In Vitro Fertilization (IVF) have to be examined for HIV, hepatitis B, and hepatitis C. If results for HIV are positive, then CD4 levels and HIV viral load need to be calculated.
• Rubella IgG testing have to be conducted. Women who’re liable to rubella must be vaccination and suggested no longer to emerge as pregnant for at least one month following vaccination.
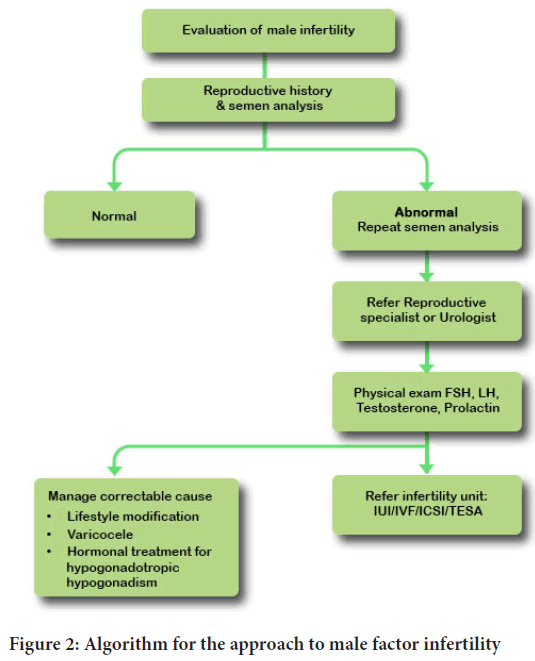
• Chlamydia screening was used for viable, STI screening and prevention should be habitual and incorporated into all fitness visits. Chlamydia antibody must bind upon the antibodies of Chlamydia trachomatis and sometimes it may not be achieved as its scientific application is limited (Figure 1).
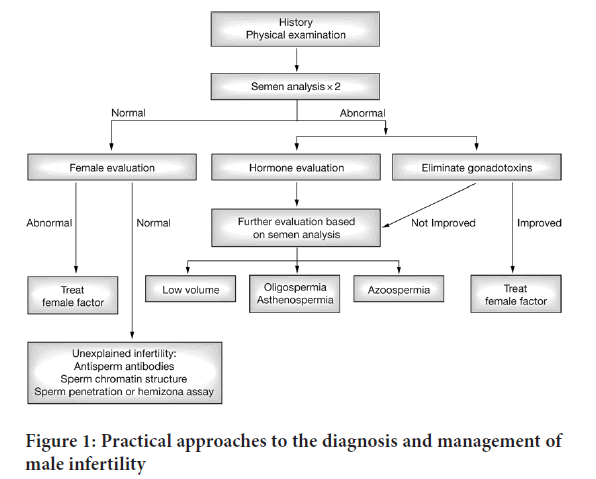
Figure 1: Practical approaches to the diagnosis and management of male infertility
Treatment and management: Nonpharmacological treatment
• Counseling must be offered earlier, at some stage before and after investigation and treatment, due to the fact fertility troubles can reason mental strain and pressure on relationships (NICE, 2013).
• Avoid intake of tobacco merchandise, illicit capsules, and immoderate alcohol.
• Avoid recreational anabolic steroids in guys as these may also have an effect on semen parameter.
• Excessive alcohol intake may additionally impair semen quality.
• Smoking impacts semen first-class and may have an impact on the threat of concept, and women and men should be counseled to prevent smoking.
• Men who’ve a high Body Mass Index (BMI) are at extended danger of infertility.
• Recreational capsules intrude with male and girl fertility, and use of anabolic steroids suppresses spermatogenesis.
Pharmacological treatment
• Medication-The use of anti-estrogens, gonadotropins (Human Chorionic Gonadotropin (HCG) and FSH), androgens, bromocriptine, or kinin-improving drug for semen abnormalities aren’t recommended because of the shortage of clinical proof for its efficacy.
• Gonadotropins-Men with hypogonadotropic and hypogonadism need to be handled with gonadotropins to hold the extent of it.
• Antioxidant therapy may be useful in idiopathic semen abnormalities.
Surgical management
• Surgery for varicoceles can be taken into consideration while there may be clinically palpable varicocele with bizarre semen parameters present, and no factor for infertility is present.
• Few cases in which IVF desires to be performed for certain elements, surgical treatment for varicoceles aren’t indicated. Vasectomy reversal must be considered in men when fertility in needed after vasectomy. Female factors should be excluded.
• Alternative remedy is testicular sperm extraction and IVF or Intracytoplasmic Sperm Injection (ICSI).
• The surgical operation has to be carried out via an experienced medical professional with the use of microsurgical method.
Assisted reproduction
• Intrauterine Insemination (IUI) is taken into consideration in some cases of moderate male component.
• Intracytoplasmic Sperm Injection (ICSI) is the encouraged remedy of preference for infertility because of male aspect. In cases of azoospermia surgical retrieval of sperm with ICSI has to be provided.
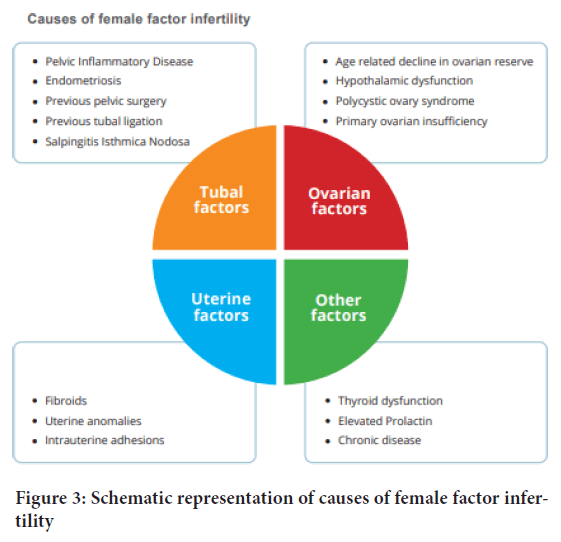
• Donor sperm is utilized in instances in which ICSI cannot be accomplished (Figure 2).
Figure 2: Algorithm for the approach to male factor infertility
Female infertility: Etiology
• Abnormal menstruation cycle
• Polycystic Ovarian Disease (PCOD)
• Cervical problems
• Endometriosis
• Structural problems
• Uterine Fibrosis
• Sexually Transmitted Diseases (STD’s)
• Hormonal imbalance
• Pelvic Inflammatory Disease
• Ovary problems
Pathophysiology
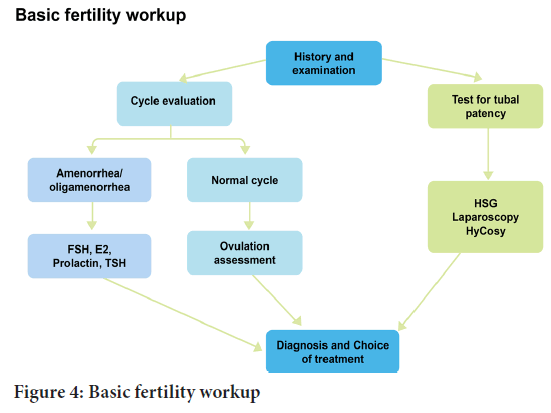
Tubal factor infertility: Blocked fallopian tubes are the maximum not a unusual reason of female infertility. It is most frequently caused by Pelvic Inflammatory Diseases (PID), endometriosis, previous pelvic surgical operation, or preceding tubal ligation.
Uterine factors: The uterus is a primary organ that could effect on reproductive outcome. Some uterine abnormalities are amenable to surgical operation that could improve the pregnant results, while some will produce positive results.
Fibroids: About 1/3 of women may have fibroids. Most fibroids do not have a bad effect on reproductive outcomes and hence require no treatment. Submucosal fibroids are mostly symptomatic and they cause heavy menstrual bleeding, prolonged menstrual cycle, implantation failure, and recurrent pregnant losses. Large intramural fibroids ranging from 5 cm or above in size need to be eliminated as they are related to poor reproductive outcome.
Uterine abnormalities: The septate uterus may additionally cause reproductive failure and an increased risk of miscarriage. Septate uterus ought to be evaluated and assess to decide if hysteroscopic removal will improve fertility outcomes. The World Health Organization (WHO) classifies ovulation disorders into three groups:
• Group I-Hypothalamic pituitary failure (hypothalamic amenorrhea or hypogonadotropic hypogonadism).
• Group II-Hypothalamic pituitary ovarian dysfunction (predominately polycystic ovary syndrome).
• Group III-Ovarian failure (Figure 3).
Figure 3: Schematic representation of causes of female factor infertility
Diagnosis
• Investigating regarding the woman reproductive age, who has no longer conceived after 1 year of unprotected vaginal sexual intercourse, in the absence of any regarded motive of infertility, has to be performed. It is recommended that couples have to be referred for counseling which must be taken into consideration in any stage of research and/or remedy due to the impact of infertility and infertility treatment (Figure 4).
Figure 4: Basic fertility workup
• Advance degrees of consultation are suitable for the woman aged ≥ 36 years. There is a recognized purpose of infertility, or a record of predisposing factors that could pose danger to fertility. This will be due to deliberate reason (as an instance: Cancer).
• Ovulation need to be confirmed with a blood test to measure serum progesterone within the mid-luteal section (day 21 of a 28-day cycle).
• Women with abnormal cycles must additionally have their gonadotropins measured. Prolactin or thyroid characteristic checks are not required however rubella reputation have to be checked and woman ought to be updated with cervical screening.
• A women age must be used as an initial predictor of her average danger of success through natural theory.
• Woman with infertility can go through ultrasonography, laparoscopy and endoscopy test to get clear view about their causes of infertility.
• There should be evaluation of hormones that include measurement of FSH (Follicle Stimulating Hormone), Luteinizing Hormone (LH), Prolactin, estrogen and progesterone.
Treatment and management: Nonpharmacological treatment
• Past medical history of women should be considered in fertility plans and recognize their lifestyle factors which play critical role in infertility (Turek PJ, 2005).
• The life factors also contribute negatively on fertility. Counseling must consist of health improving practices and lifestyle modification. The following are primarily based prevention techniques for infertility: Safe sexual practices and prevention of Sexually Transmitted Infection (STI) with screening for STI at each session.
• Maintaining a wholesome weight-There is evidence that each female and male fertility are decreased through being either obese with a Body Mass Index (BMI) of >25 kg/m² or underweight with a BMI <20 kg/m².
• Avoid exposure to tobacco products, illicit drugs, and excessive alcohol.
Pharmacological treatment
• Dopamine agonist-Women with ovulatory issues due to hyper prolactinemia are given dopamine agonist which includes bromocriptine.
• Surgery-For women with moderate tubal sickness, tubal surgical treatment may be greatly effective than no remedy.
• Hysteroscopic acheilia’s-Women with amenorrhea and intrauterine adhesions are provided with hysteroscopic adhesiolysis due to the fact that this restores menstruation and enhance the risk of being pregnant.
• Women intending to become pregnant need to intake nutritional supplementation with folic acid earlier than thought and as much as 12 weeks’ before gestation reduces the chance of having a baby with Neural Tube Defects (NTD). The endorsed dose is 0.4 mg for women who formerly had a toddler with a Neural Tube Defect or who are receiving anti-epileptic remedy or who’ve diabetes.
• Preconception counseling is critical to all women searching for fertility treatment to optimize pregnancy consequences. The counseling has to be in accordance with the WHO preconception care package deal of preconception care interventions.
• Maternal age-Women over 35 years of age, who’re asking for fertility treatment need to consider the dangers of pregnancy with superior maternal age.
• Folic acid supplementation is vital to reduce unfavorable pregnant consequences. Folic acid supplementation before minimum two months and 12 weeks gestation reduces the risk of Neural Tube Defects (NTD) within the toddler. Evidence-based studies totally suggest for folic acid supplementation.
• Women who do not have risk factors for NTDs have to take 400 μg (or 0.4 mg) of folic acid per day. Women at excessive danger of NTD’s have to be diagnosed and who have had a previous pregnancy with Neural Tube Defect, have a family history of Neural Tube Defects, who are receiving antiepileptic tablets/folate antagonists (e.g: Methotrexate, sulphonamides, dolutegravir), having malabsorption issues (e.g: Inflammatory bowel ailment) and having weight problems with BMI>35 kg/m2 have diabetes.
• Women at immoderate threat have to be supplied with high-dose supplementation (5 mg folic acid every day) and recommended to increase their meals consumption with folic acid.Risk factors associated with both males and females
• Chlorine: Chlorine not only damage natural fertility but also makes in vitro fertilization much less likely to succeed. The worst fertility disrupters are organochlorine compounds. Sometimes, the reaction results in chlorination byproducts such as chloramines which can damage men’s testes and disrupt sperm development (Talaiekhozani A, et al ., 2016).
• Pesticides: Pesticides are harmful to the reproductive system which sometimes damage cell that are responsible for fertility. Pesticide exposure also been implicated in miscarriage, premature birth, altered sex ratio and reduced fertility rate. High level of pesticide residue in fruits and vegetables can lower sperm count in men.
• Anabolic steroids: Anabolic steroids in males can lead to impotency, reduction in sperm production in testicles. In case of female there is reduction of estrogen, progesterone, Luteinizing Hormone and Follicle Stimulating Hormone (Balen AH, et al ., 2016).
• X-rays: High exposure to x-rays diminishes egg production and quality in females and it also affects uterus and cervix. In males it reduces sperm production.
• Mobile/laptop: Cell phones decreases the semen quality, also decreases sperm count, motility and normal morphology. Long time exposure to cellular radiation leads to infertility and affects normal activity of ovaries in females.
• Water quality: Low quality of water leads to hormone disruption that leads to hormonal imbalance and causes infertility.
• Caffeine: Higher intake of caffeine i.e. coffee or tea increase risk of miscarriage and decrease sperm quality.
• Preservatives: Parabens are inexpensive and effective preservative found in many personal care and foods which is endocrine disruptors which alters hormonal function in the human body.
• Addiction: Alcohol can alter sperm count, size, shape and motility. It lowers the levels of LH, FSH and Testosterone and raise level of estrogen which reduce sperm production. In females, there are changes in ovulation and cycle regulation.
• High temperature: Exposure to high temperature cause lower sperm production due to death of sperm cells. It also decreases fertility rate.
Discussion and Conclusion
Infertility is classified as primary and secondary infertility. Primary infertility is inability to have pregnancy and secondary is inability to have a pregnancy after previously successful conception. However, environmental and lifestyle factors such as smoking, excessive alcohol intake, obesity and exposure to environmental pollutants is also associated with lower fertility rates. People affected by this condition have higher rates of depression, anxiety, suicide, divorces, intimate partner violence and social problems. There are many factors that are responsible for infertility. Main causative factors are male and female factors. Apart from this there are also other factors such as a combination of male and female factors, Environmental factors, Social factors, Nutritional factors, Sexually Transmitted Infection (STI), Genetic factors and lifestyle factors like smoking, excessive alcohol intake, obesity and exposure to environmental pollutants.
References
- WHO. Infertility. World Health Organization. 2020.
- Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: A systematic analysis of 277 health surveys. PLoS Med. 2012; 9(12): e1001356.
[Crossref] [Google Scholar] [Pubmed]
- Rastogi A. Infertility. National Health Portal of India. 2016.
- NDP. National Clinical Guidelines for Safe Conception and Infertility. National Department of Health, Republic of South Africa. 2019.
- NICE. Fertility problems: Assessment and treatment. National Institute of Healthcare and Care Excellence. 2013.
- Turek PJ. Practical approaches to the diagnosis and management of male infertility. Nat Clin Pract Urol. 2005; 2(5): 226-238.
[Crossref] [Google Scholar] [Pubmed]
- Talaiekhozani A, Alaee S, Ziaei GR, Mir M, Yazdan M, Ataabadi MS. Knowledge of men and women about infertility risk factors. Iran J Health Saf Environ. 2016; 3(4): 600-606.
- Balen AH, Morley LC, Misso M, Franks S, Legro RS, Wijeyaratne CN, et al. The management of anovulatory infertility in women with polycystic ovary syndrome: an analysis of the evidence to support the development of global WHO guidance. Hum Reprod Update. 2016; 22(6): 687-708.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Chaudhari Hiral Shankarbhai1*, Dhiren L Chaudhari1 and Jalpa A Soni22Department of Pharmacology, Arihant College of Pharmacy, Gujarat, India
Citation: Shankarbhai CH: Causative Factors, Diagnostic Testing and Management of Infertility
Received: 27-Apr-2023 Accepted: 22-May-2023 Published: 29-May-2023, DOI: 10.31858/0975-8453.14.5.296-300
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3