Case Report - (2022) Volume 13, Issue 1
Abstract
The authors presented a case of a combination of chronic dacryocystitis and Silent Sinus Syndrome in a 69-year-old female patient with long-term lacrimation and facial deformity. Thus, even such rare diseases can occur in patients of the older age group.
Keywords
Silent sinus, Dacryocystitis, Enophthalmos, Nasolacrimal ducts, Case report
Introduction
Dacryocystitis is an infectious inflammatory disease of the lacrimal sac. It can be acute or chronic as well as congenital or acquired. As a rule, acute dacryocystitis is marked by a sudden onset of pain, redness, swelling in the region of the lacrimal canal, lacrimation, and sometimes suppuration. A common serious complication of acute dacryocystitis is phlegmon (Cohen AJ, et al., 2006).
In chronic dacryocystitis, a frequent symptom is lacrimation occurring due to impaired tear clearance. This, in turn, can be aggravated by conjunctivitis which occurs as a result of exposure to exotoxins secreted by the microflora normally present on the eye surface and cannot be removed in a natural way due to impaired tear clearance (Bartley GB, 1992).
Acquired dacryocystitis is caused by obstruction in the lower part of the nasolacrimal ducts. As a matter of fact, there are often comorbid pathologies in the ENT organs, such as: Inferior turbinate hypertrophy; a deviated nasal septum; nasal polyps; allergic, hypertrophic and vasomotor rhinitis; sinusitis (maxillary sinusitis, ethmoiditis); traumatic injuries; tumors in the nose and ethmoid sinuses. These pathologies can also be somewhat conducive to dacryocystitis (Corey JP, et al., 1993).
Late treatment often leads to serious complications. Obstruction of the lacrimal canals and large accumulation of fluid causes an abscess or phlegmon. They, in turn, tend to promote the development of complications in the regions of the brain. Chronic dacryocystitis can contribute to the manifestation of meningitis or purulent encephalitis.
The Silent Sinus Syndrome (SSS) is a relatively uncommon disease. Clinical manifestations of this condition were first described as “two cases of enophthalmos associated with ‘mucocele’ of the maxillary sinus” in 1964, but only by 1994, Soparkar CN, et al. proposed to introduce the SSS term, giving a detailed description of this complex of symptoms drawing on the case of 19 patients they observed (Montgomery W, 1964; Soparkar CN, et al., 1994). According to their definition, the syndrome includes the spontaneous development of progressive enophthalmos and hypophthalmos that arise secondarily because of hypoplasia of the maxillary sinus on the ipsilateral side and the resorption of the orbital bone that develops as its volume increases correspondingly. Radiographic imaging reveals a partial decrease in, or a total absence of pneumatization in the corresponding sinus. It should be emphasized that for this condition, a complete absence of subjective symptoms of chronic sinusitis is characteristic. The patient reports no facial pain or feeling of pressure in the area of the maxillary sinus projection that would be associated with increasing facial asymmetry. This characteristic lack of subjectively perceived symptoms is the main criteria for differential diagnosis against another similar condition, Chronic Maxillary Atelectasis (CMA).
Kass et al. described CMA in 1997 as “a persistent decrease in the volume of the maxillary sinus associated with the bending of the interior of its walls” (Salman S, et al., 1997). The authors broke the development of this condition into 3 distinct stages:
• Stage I (membranous deformity) is defined by lateralization of the fontanella sinus maxillaris.
• Stage II (bone deformity) is characterized by the emergence of a bend in the interior of one or more walls of the sinus.
• Stage III (clinical deformity) displays pronounced clinical manifestations, accompanied by the emergence of enophthalmos, hypophthalmos and the deformation of the proportions of the midface zone caused by these conditions.
In addition, the vast majority of patients had symptoms of chronic maxillary sinusitis. Using these criteria, patients with the SSS can be conditionally classified as having Stage III CMA; however, in specialist literature, this question is still being debated. In some cases, differential diagnosis is quite difficult, especially in children. This is explained by the fact that in patients of this age group, one frequently observes hypertrophied adenoid vegetations causing clinical symptoms. At the same time, they do not display the classic manifestations of maxillary sinusitis (Brandt MG and Wright ED, 2008). Children also get SSS-related headaches more often than adults do (Farneti P, et al., 2017). Due to the difficulty of differential diagnosis and based on the data in specialist literature, most authors are inclined to believe that the SSS should be recognized as a special case of Stage III CMA (Brandt MG and Wright ED, 2008; Gunaratne DA, et al., 2016).
Historically, the SSS has been described as a pathology that develops on one side, and has mostly been observed to develop on the right (in up to 72% cases), which is likely explained by small sample size (Soparkar CN, et al., 1994; Gunaratne DA, et al., 2016). However, there have been reports of clinical cases of the SSS and CMA on both sides (Trope M, et al., 2017; Ferri A, et al., 2012; de Dorlodot C, et al., 2017), and this is reason enough to reconsider the well-established classic definition. This condition commonly develops when the patient is between 30 and 60 years old, and there is no difference in its occurrence rate gender-wise (Gunaratne DA, et al., 2016).
Case Presentation
Etiology
The etiology of the development of these syndromes has yet to be thoroughly studied. As a triggering factor, conditions predisposing to chronic hypoventilation of the maxillary sinus have been suggested as likely candidates. Specifically, one of them is a spontaneously developing lateralization of the uncinate process, a condition that contributes to the emergence of the “valve effect” (Gunaratne DA, et al., 2016; Hobbs CG, et al., 2004). Other reasons behind the development of secondary atelectasis are:
• Anatomical variations (for example, a deviated nasal septum, concha bullosa, paradoxically curved middle turbinate), chronic inflammatory process in the ostiomeatal complex (Blackwell KE, et al., 1993),
• Post-traumatic changes in the region of the ostiomeatal complex and the medial wall of the orbit (Pawar SS, et al., 2010),
• Foreign body presence (Fidan V, 2008),
• Occlusion of the anastomosis by adipose tissue after medial decompression of the orbit (Rose GE and Lund VJ, 2003),
• Benign neoplasms of the nasal cavity (Hens G, et al., 2005).
Chronic hypoventilation and impaired outflow of secretion by way of natural anastomosis cause a decrease in pressure within the sinus, and viscous mucous discharge begins to accumulate in it. In terms of its mechanism of emergence, this process is to some extent comparable with the main stages of development of secretory otitis media. If the process is prolonged, the sinus bone walls begin to display signs of osteolysis due to increased osteoblast activity in a low-pressure environment and chronic indolent inflammation (Salman S, et al., 1997). Thinner sinus walls, in turn, are more easily retracted. As the upper wall of the maxillary sinus lowers, the volume of the orbital cavity increases (Gunaratne DA, et al., 2016; Kass ES, et al., 1996; Wan MK, et al., 2000).
It should be noted that in children, if the sinus anastomosis is occluded, it can contribute to the initial hypoplastic development of the sinus with the emergence of CMA (Farneti P, et al., 2017).
Diagnosis
The fact that the SSS is such a rare diagnosis may be partly due to it being underdiagnosed. For a considerable period, patients have no complaints or clinical symptoms. Because of that, patients start seeking medical assistance mostly at later stages, when the lower wall of the orbit lowers so significantly that the patient develops diplopia. It is also then that a noticeable cosmetic defect appears when the affected eye shrinks visibly compared to the other eye, the upper orbital sulcus deepens and the midface region becomes visibly asymmetric. Occasionally, a (pseudo-?) retraction of the upper and lower eyelids develops, lagophthalmos occurs, and/or the mobility of the eyeball is impaired. The first medical specialist to observe such a patient is often an ophthalmologist who is not always able to establish the correct diagnosis. Much less frequently, the SSS is revealed at the stage preceding the development of clinical symptoms, when the patient undergoes an MSCT (Multi Sliced Computed Tomography) or MRI (Magnetic Resonance Imaging) scan of the head related to another disease. In this case, the otorhinolaryngologist notices signs of atelectasis of the maxillary sinus while its anastomosis is blocked; the sinus will usually appear totally darkened. As to patients with CMA, because they display clinical symptoms of chronic maxillary sinusitis, in theory, they are more often diagnosed at an earlier stage by an otorhinolaryngologist.
On an MSCT scan of the paranasal sinuses, the following characteristic features can be found: Lowering of the bottom of the orbit coupled with an increase in its volume; a concomitant decrease in the volume of the maxillary sinus while its bone walls are retracted and thinned; and a total or subtotal decrease in its pneumatization (Gunaratne DA, et al., 2016).
It is characteristic to observe a lateralization of the uncinate process and, often, of the adjacent part of the middle turbinate along with the occlusion of the ostiomeatal complex.
Treatment
When the first descriptions of this syndrome were published, the condition was most often treated via the radical Caldwell-Luke operation. Currently, the surgical treatment gold standard for it is endoscopic rhinoanthrostomy in the middle nasal passage. This method is considered effective because it efficiently eliminates the block in the natural anastomosis of the sinus, which is the main cause of the development of the syndromes. The question of whether it is necessary to reconstruct the lower wall of the orbit remains controversial. If so, it must also be determined whether these two distinct treatment stages should be performed simultaneously, or the second stage should happen 6 months after the first surgical intervention. Most authors conclude that it is sufficient to eliminate the cause of this condition, and that on its own will cause its clinical manifestations to regress partially. Subsequently, if necessary, the bottom of the orbit can be reconstructed as second stage surgery, provided there are indications for it, i.e., if ophthalmic symptoms persist and the cosmetic deformity is significant (Brandt MG and Wright ED, 2008; Farneti P, et al., 2017; Gunaratne DA, et al., 2016; Babar-Craig H, et al., 2021). Less often, cases of simultaneously carrying out these operations have been described; in this case, the orbit is accessed sub-or transconjunctivally (Cardesín A, et al., 2013; Bossolesi P, et al., 2008; Yip CC, et al., 2003). The most reasonable tactic, according to the authors, is the first of the above: Firstly, significant regression of clinical manifestations is possible even after first stage surgery; secondly, the risk of infecting the orbital structures is relatively low.
Clinical observation
Patient A, 69 year old complained of facial asymmetry, namely a decrease in the size of the left eye in comparison with the right one and enophthalmos of the left eye, along with lacrimation. These symptoms arose spontaneously-the patient denies a prior trauma.
The patient reported having experienced left eye lacrimation over the period of 10 years. She had repeatedly consulted ophthalmologists but every time was prescribed conservative therapy: Steroid anti-inflammatory drops and anti-allergic ophthalmic agents. However, lacrimation persisted. The patient did not present other complaints characteristic of dacryocystitis, such as purulent discharge from the eye, painful sensations, and “tingling” in the eye area and lacrimal sac swelling, all of which could have delayed the correct diagnosis (Figure 1a).
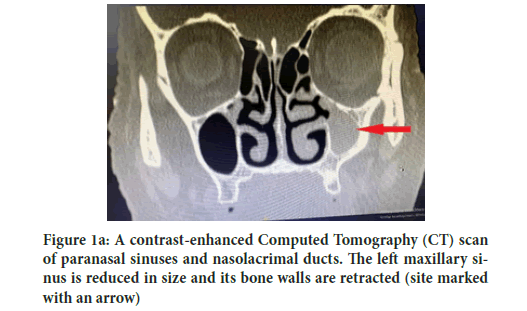
Figure 1a: A contrast-enhanced Computed Tomography (CT) scan of paranasal sinuses and nasolacrimal ducts. The left maxillary sinus is reduced in size and its bone walls are retracted (site marked with an arrow)
The patient did not seek help from otorhinolaryngologists regarding these complaints since there were no complaints pertaining to the ENT (Ear, Nose and Throat) organs. Only in July 2019 was the patient referred to an ENT doctor who recommended taking a contrast-enhanced Computed Tomography (CT) scan of the paranasal sinuses and the lacrimal apparatus (with Omnipaque serving as a contrasting agent) (Figure 1b).
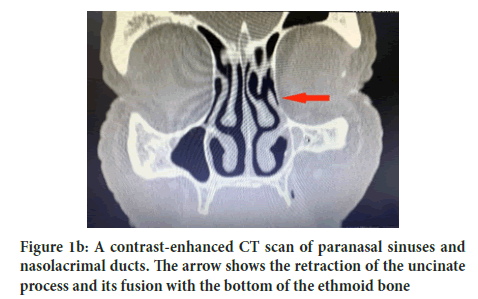
Figure 1b: A contrast-enhanced CT scan of paranasal sinuses and nasolacrimal ducts. The arrow shows the retraction of the uncinate process and its fusion with the bottom of the ethmoid bone
The cervix of the left lacrimal sac is narrowed to 0.3 mm. In the left maxillary sinus, the uncinate process visibly fuses with the bottom of the ethmoid bone. The left maxillary sinus is reduced in size. The superior and anterior bone walls of the sinus are retracted. The left upper part of the sinus is completely filled with homogeneous contents. The other paranasal sinuses are pneumatized (Figure 1c).
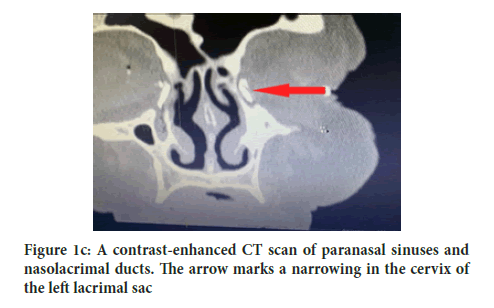
Figure 1c: A contrast-enhanced CT scan of paranasal sinuses and nasolacrimal ducts. The arrow marks a narrowing in the cervix of the left lacrimal sac
Results and Discussion
As a result of a series of examinations, namely an endoscopic examination of the nasal cavity, an ophthalmological examination and a CT scan of the paranasal sinuses and the lacrimal apparatus, the patient was diagnosed with the following: Left-sided chronic maxillary sinusitis; the Silent Sinus Syndrome; left-sided chronic dacryocystitis. With a view to these diagnoses, it was decided to treat these conditions surgically (Figure 2).
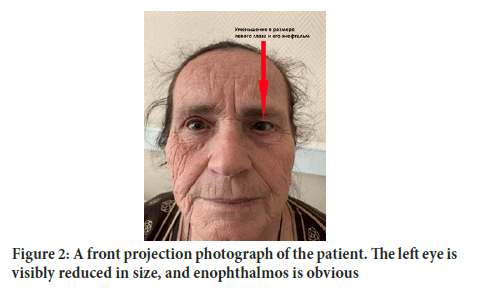
Figure 2:A front projection photograph of the patient. The left eye is visibly reduced in size, and enophthalmos is obvious
The patient underwent endoscopic surgery on the left maxillary sinus with simultaneous dacryocystorhinostomy. The surgery was performed under endotracheal anesthesia. The nasal passage was generally examined using an endoscope, and the middle turbinate was visualized. Additional infiltration anesthesia of the mucous membrane was administered, and the middle turbinate was deflected to the left; after that, the retracted uncinate process was identified. Using reverse cutting forceps, the horizontal part of the uncinate process was resected. The natural anastomosis of the upper part of the sinus was expanded and the sinus was examined, revealing a pronounced retraction of the anterior and superior bone walls. Also, thick mucin was present, and it was aspirated. At the second stage of the surgery, using a radio wave scalpel (30 W), an incision in the shape of an inverted U was made in the mucous membrane in the projection of the lacrimal sac, and the flap was separated. With the help of a bur and the Kerrison rongeur, the medial bone wall of the lacrimal sac was removed, and the sac cavity was opened. No purulent discharge was obtained. A wide canal was created between the lacrimal sac and the nasal cavity. The excess mucous membrane was removed using 45° scissors and Blakesley forceps. Fragments of a hemostatic sponge were installed in the cavity of the sac and in the middle nasal passage. Monitoring was performed by probing the lacrimal system through the inferior lacrimal canaliculus. A tampon was introduced into the middle nasal passage on the left and was then removed after 2 days. The patient responded satisfactorily to surgical treatment. In the postoperative period, she was administered conservative treatment (cleaning the nasal cavity, administering anti-inflammatory therapy in the form of corticosteroid ophthalmic drops with an antibacterial effect, and rinsing the left maxillary sinus and nasolacrimal ducts).
The patient was discharged on the 5th day after the surgery in a satisfactory condition for outpatient follow-up treatment under dynamic supervision.
Conclusion
The Silent Sinus Syndrome is a rare and poorly diagnosed condition. The gold standard for diagnosis is a CT scan of the paranasal sinuses. If left untreated, a long-term Silent Sinus Syndrome can cause obstruction of the nasolacrimal ducts. Combination of chronic dacryocystitis and Silent Sinus Syndrome with long-term lacrimation and facial deformity is such a rare disease that can occur in patients of the older age group. The patient underwent endoscopic surgery on the left maxillary sinus with simultaneous dacryocystorhinostomy.
Consent to Participate
The patient’s informed consent was obtained and their medical data were used for research.
References
- Cohen AJ, Brazzo BG, Mercandetti M. The lacrimal system: Diagnosis, man and surgery. Springer. 2006.
- Bartley GB. Acquired lacrimal drainage obstruction: An etiologic classification system, case reports, and a review of the literature-Part 1, 2, 3. Ophthal Plast Reconstr Surg. 1992; 8(4): 237-242.
[CrossRef] [Google scholar] [Pubmed]
- Corey JP, Bumsted R, Panje W, Namon A. Orbital complications in functional endoscopic sinus surgery. Otolaryngol Head Neck Surg. 1993; 109(5): 814-820.
[CrossRef] [Google scholar] [Pubmed]
- Montgomery W. Mucoceles of the maxillary sinus causing enophthalmos. Eye Ear Nose Throat Mon. 1964; 43: 41-44.
- Soparkar CN, Patrinely JR, Cuaycong MJ, Dailey RA, Kersten RC, Rubin PA, et al. The silent sinus syndrome: A cause of spontaneous enophthalmos. Ophthalmology. 1994; 101(4): 772-778.
[CrossRef] [Google scholar] [Pubmed]
- Salman S, Weber AL, Kass ES, Rubin PA, Montgomery WW. Chronic maxillary atelectasis. Ann Otol Rhinol Laryngol. 1997; 106(2): 109-116.
[CrossRef] [Google scholar] [Pubmed]
- Brandt MG, Wright ED. The silent sinus syndrome is a form of chronic maxillary atelectasis: A systematic review of all reported cases. Am J Rhinol. 2008; 22(1): 68-73.
[CrossRef] [Google scholar] [Pubmed]
- Farneti P, Sciarretta V, Macrì G, Piccin O, Pasquini E. Silent sinus syndrome and maxillary sinus atelectasis in children. Int J Pediatr Otorhinolaryngol. 2017; 98: 150-157.
- Gunaratne DA, Hasan Z, Floros P, Singh N. Bilateral stage I chronic maxillary atelectasis: A case report. Int J Surg Case Rep. 2016; 26: 53-56.
- Trope M, Schwartz JS, Tajudeen BA, Kennedy DW. Bilateral silent sinus syndrome: A rare case and review of literature. Allergy Rhinol. 2017; 8(2): 100-102.
[CrossRef] [Google scholar] [Pubmed]
- Ferri A, Ferri T, Sesenna E. Bilateral silent sinus syndrome: Case report and surgical solution. J Oral Maxillofac Surg. 2012; 70(1): 103-106.
- De Dorlodot C, Collet S, Rombaux P, Horoi M, Hassid S, Eloy P. Chronic maxillary atelectasis and silent sinus syndrome: Two faces of the same clinical entity. Eur Arch Otorhinolaryngol. 2017; 274(9): 3367-3373.
[CrossRef] [Google scholar] [Pubmed]
- Hobbs CG, Saunders MW, Potts MJ. Spontaneous enophthalmos: Silent sinus syndrome. J Laryngol Otol. 2004; 118(4): 310-312.
[CrossRef] [Google scholar] [Pubmed]
- Blackwell KE, Goldberg RA, Calcaterra TC. Atelectasis of the maxillary sinus with enophthalmos and midface depression. Ann Otol Rhinol Laryngol. 1993; 102(6): 429-432.
- Pawar SS, Hong S, Poetker DM. Delayed presentation of silent sinus syndrome after orbital trauma. Am J Otolaryngol. 2010; 31(1): 61-63.
[CrossRef] [Google scholar] [Pubmed]
- Fidan V. Silent sinus syndrome associated with nasal foreign body. Int J Pediatr Otorhinolaryngol Extra. 2008; 3(2): 75-77.
- Rose GE, Lund VJ. Clinical features and treatment of late enophthalmos after orbital decompression: A condition suggesting cause for idiopathic “imploding antrum”(silent sinus) syndrome. Ophthalmology. 2003; 110(4): 819-826.
[CrossRef] [Google scholar] [Pubmed]
- Hens G, Hermans R, Jorissen M. Chronic maxillary atelectasis. B ENT. 2005; 1: 25.
- Kass ES, Salman S, Montgomery WW. Manometric study of complete ostial occlusion in chronic maxillary atelectasis. Laryngoscope. 1996; 106(10): 1255-1258.
[CrossRef] [Google scholar] [Pubmed]
- Wan MK, Francis IC, Carter PR, Griffits R, van Rooijen ML, Coroneo MT. The spectrum of presentation of silent sinus syndrome. J Neuroophthalmol. 2000; 20(3): 207-212.
- Babar-Craig H, Kayhanian H, de Silva DJ, Rose GE, Lund VJ. Spontaneous silent sinus syndrome (imploding antrum syndrome): Case series of 16 patients. Rhinology. 2011; 49(3): 315.
[CrossRef] [Google scholar] [Pubmed]
- Cardesín A, Escamilla Y, Romera M, Molina JA. Single surgical step for endoscopic surgery and orbital reconstruction of a silent sinus syndrome. Acta Otorrinolaringol. 2013; 64(4): 297-299.
[CrossRef] [Google scholar] [Pubmed]
- Bossolesi P, Autelitano L, Brusati R, Castelnuovo P. The silent sinus syndrome: Diagnosis and surgical treatment. Rhinology. 2008; 46(4): 308.
- Yip CC, McCulley TJ, Kersten RC, Tami TA, Kulwin DR. Silent sinus syndrome as a cause of diplopia in a child. J Pediatr Ophthalmol Strabismus. 2003; 40: 309-311.
[CrossRef] [Google scholar] [Pubmed]
Author Info
V M Svistushkin1, Liana S Karapetyan1*, N N Krakhovetsky2, T K Shadyev1 and S V Starostina12Department of Lacrimal Pathology, Federal State Budgetary Institution of Science,Research Institute of Eye Diseases, Moscow, Russia
Received: 13-Dec-2021 Accepted: 27-Dec-2021 Published: 03-Jan-2022, DOI: 10.31858/0975-8453.13.1.38-41
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






