Research Article - (2021) Volume 12, Issue 12
Delays in the Surgical Pathway in Breast Cancer Patients in Tunisia: A Descriptive Prospective Study
Kahlaoui Meriam1*, Limam Manel1, Sahli Jihene1, Khairi Hédi2, Mtiraoui Ali1 and Ajmi Thouraya1Abstract
Objectives: Describe the surgical pathway and identify the different waiting times to surgery of women with a breast cancer in the Gynecology Department of the University Hospital of Sousse in Tunisia.
Methods: It is a descriptive prospective study based on an assessment of professional practices using the process approach method. The study focused on the surgical management of women with breast cancer followed and scheduled for surgical treatment. The data were collected using a data collection sheet, developed according to a literature review.
Results: The sample consisted of 77 women. Ten waiting times have been calculated. Global time to first treatment (surgical treatment) was 78.5 days with an Interquartile range (IIQ) of [55.5-113.25 days]. The information period was 10 days with an IIQ of [3-19 days]. The global time of access to surgery was 43.5 days with an IIQ of [40-54.75].
Conclusion: Delays in access to care appear to be a potential marker of inequalities in access to care and an indicator of the performance of the health care system and can influence patient prognosis. The reduction of these delays must be integrated into a continuous quality improvement approach.
Keywords
Breast cancer, Patient care management, Waiting time, Surgical pathway, Delays
Introduction
Cancer constitutes an enormous burden on society in both more and Less Economically Developed Countries (respectively MEDCs and LEDCs) and becomes the second leading cause of death in the world (Torre LA, et al., 2015). Globally, about one in six deaths is due to cancer (WHO, 2010; WHO, 2018). Breast cancer is the most common cancer diagnosed in women worldwide and is the major cause of cancer death among this group (WHO, 2010; WHO, 2018), making it a global public health issue. In Tunisia, breast cancer is also the leading cancer in women representing 30% of all female cancers. Its incidence in 2017 is estimated at 50.17/100000 persons years, and is still increasing on rise and the diagnosis is still made late (Cherif A, et al., 2019). In fact, the average clinical tumor size at the time of diagnosis exceeds 4 cm with an average consultation time of six months. More than half of the women are diagnosed at a locally advanced (40%) or metastatic stage (15%), resulting in a poor outcome in terms of survival (Ministry of Health, 2020; Landolsi A, et al., 2010).
Since the incidence of breast cancer is rising, there has been growing awareness of delays in accessing care (Molinié F, et al., 2013). In oncology, the complexity of care trajectories results in inequalities of care access, particularly in terms of waiting time. These delays depend on three factors; the patient factors, healthcare professionals and the healthcare system in general. Waiting times may vary depending on the country, the region, the characteristics of the patient, the type of cancer and the management strategy (Pourcel G, et al., 2013). In several countries, the waiting time to access healthcare services has become a priority in public health policies (Revaux A, et al., 2014). This measure is a key element in the quality and continuity of care. It is also a performance indicator of the healthcare system and a tracer of inequalities in access to healthcare (Molinié F, et al., 2013). Previous research has shown that timely diagnosis and treatment of breast cancer can improve survival outcomes (Bleicher RJ, et al., 2016; Webber C, et al., 2020). Most women diagnosed with breast cancer will undergo surgery as part of their treatment. Surgery, a common first line treatment option in breast cancer, has a crucial diagnostic, therapeutic and prognostic role. Surgical treatment delays can lead to consequential delays in post-operative chemotherapy or radiation therapy. More specifically, it has been shown recently that surgery delays can also affect survival rate even for early stage breast cancer (Bleicher RJ, et al., 2016). Avoiding delays in breast cancer treatment is obviously crucial to ensure the best possible outcomes (Colleoni M, et al., 2000; Shin DW, et al., 2013). Unfortunately there is no consensus defining an acceptable timeframe specifying how soon a patient should undergo surgery after diagnosis (Shin DW, et al., 2013). For these reasons it is essential to have a good control of waiting times during the treatment process in order to guarantee the best clinical outcomes for patients diagnosed with breast cancer. In this context, we have carried out this study as part of a quality improvement project at the department of Gynecology in the Region of Sousse. Our objectives were to describe surgical pathway followed by women diagnosed with breast cancer in order to estimate waiting times in each step and to identify potential dysfunctions in this process.
Methods
Study design and population
We conducted a prospective descriptive study among patients monitored and scheduled for surgical treatment of breast cancer at the Department of Gynecology of Sousse-Tunisia. We excluded in this study males with breast cancer and women with breast cancer which surgery was proposed in the second- line (after neoadjuvant chemotherapy or radiotherapy). The patients included in our sample were recruited over a period of two months (February and March, 2017) from the weekly surgical multidisciplinary team discussion. The women were accompanied and followed during all the stages of the care pathway.
Measuring instrument and data collection
The data were collected using an anonymous data collection sheet developed for the purpose of this study. This sheet was designed to follow the surgical pathway of women diagnosed with breast cancer using the method of process which describe in details all the stages of the process undergoing by the patient and calculate at the same time the different waiting times.
In order to obtain the different data and dates for each patient, different document have been consulted (medical files, department registers, etc.) as well as interviews with healthcare professionals and administrative staffs involved in the process.
Operational definitions of variables
The measuring and the selection of the different times from the first contact with the health care system to treatment were based on their availability, after a review of the literature. The waiting times studied were:
The global waiting times
• The global waiting time to first treatment (surgery): Time between the radiological diagnosis and the onset of the surgery.
• The first intermediate time (the waiting time to access to diagnosis): Time between the radiological diagnosis and the pathological diagnosis (Anatomopathological results).
• The second intermediate time (the waiting time to access to first treatment (surgery)): Between the time of pathological diagnosis (Anatomopathological results) of the breast cancer and the onset of the surgery.
The different waiting times of the surgical pathway of women with breast cancer
• The appointment waiting time (1): Is the time between the day which the patient is presented to the reception to make an appointment and the date of the first consultation (Figure 1).
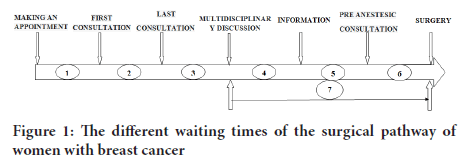
Figure 1: The different waiting times of the surgical pathway of women with breast cancer
• The waiting time to diagnosis (2): Is the time between the first consultation and the last consultation before the multidisciplinary discussion (formulation of the diagnosis).
• The waiting time to the multidisciplinary discussion (3): Is the time between the last consultation and the multidisciplinary discussion date.
• The information period (4): Is the period between the multidisciplinary discussion (during which the final decision of the diagnosis and the nature of the surgical procedure is confirmed) and the date of the receipt of the information by the patient.
• The waiting time to the pre-anesthetic consultation (5): Is the time between the receipt of the information and the pre-anesthetic consultation.
• The waiting time to surgery (6): Is the time between the pre-anesthetic consultation and the surgery.
• The global waiting time of access to surgery (7): Is a global waiting time between the multidisciplinary discussion during which the decision is made (date of the decision to treat) and surgery (treatment).
This timeframe can give us an overall picture of the waiting time and the delays between the announcement of the decision of surgery (the decision to treat) and the surgery.
Statistical analysis
Data entry and analysis were performed using SPSS 21.0 software. The normality of the quantitative variables was verified with the Kolmogorov Smirnov test. When the variable was normally distributed, it was described with its mean and its standard deviation, otherwise with the median and Interquartile ranges. The qualitative variables were described with number and percentages.
Results
Breast cancer surgical pathway
Data collection and personalized accompaniment for women with breast cancer into the surgical pathway allowed us to schematize this surgical pathway in the form of a flowchart, which begins with the entry of the woman with breast cancer, until the exit of the woman after a surgery for breast cancer (Figure 2).
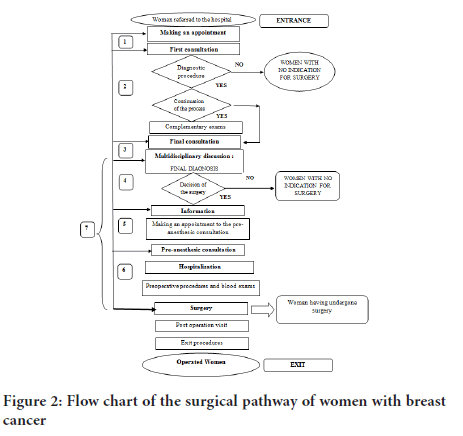
Figure 2: Flow chart of the surgical pathway of women with breast cancer
Socio-demographic characteristics of patients and the mode of discovery
We included 77 women. The mean age was 46, 8 ± 13,9 years of which 66,2% were married (n=51/77). Nearly one third of the patients had a primary education (36,4%). More than half of the women were unemployed (59,7%). The most common mode of discovery that revealed the anomaly was self-examination in 50,6% of cases (Table 1).
| Number(n) | Percentage(%) | |
|---|---|---|
| Family situation | ||
| Single | 15 | 19,5 |
| Married | 51 | 66,2 |
| Divorcee | 2 | 2,6 |
| Widow | 9 | 11,7 |
| Level of the study | ||
| Illiterate | 26 | 33,8 |
| Primary | 28 | 36,4 |
| Secondary | 12 | 15,6 |
| University | 11 | 14,3 |
| Profession/Activity | ||
| Student | 5 | 6,5 |
| Not working patient | 46 | 59,7 |
| Working patient | 26 | 33,8 |
| Discovery mode | ||
| Palpation (self-examination) | 39 | 50,6 |
| screening | 16 | 20,8 |
| Imaging | 22 | 28,57 |
| Mammography done before the consultation | 75 | 97,4 |
| Biopsy done before the consultation | 29 | 37,6 |
Table 1: Sociodemographic characteristics and mode of discovery
General characteristics of the care
In total, of the 77 women that were staffed and scheduled for surgery among 56 (72,7%) underwent the operation and the rest n=21(27,3%) of women did not undergo the surgery as they were absent the day of the surgery for unknown reasons.
The majority of the patients (40,3%) needed only one consultation before the multidisciplinary discussion. Regarding the act retained after the multidisciplinary discussion, for the majority of cases (n=55; 71,4%) it was a conservative surgery. In reference to the information, 87% of the patients were informed about the date of the surgery. The information was provided in 100% of cases by the nurse (Table 2).
Number(n) |
Percentage(%) |
|
|---|---|---|
Number of consultations before the final diagnosis |
||
One consultation |
31 |
40,3 |
Two consultations |
28 |
36,4 |
Over two consultations |
18 |
23,3 |
Breast surgery type |
||
Conservative |
55 |
71,4 |
Radical |
22 |
28,6 |
Information |
||
Yes |
67 |
87 |
No |
10 |
13 |
Method of information (n=67) |
||
By telephone |
25 |
37,3 |
Presenting in the service |
42 |
62,7 |
The person who informed the patient |
||
By the nurse |
67 |
100 |
By the doctor |
0 |
0 |
Hospitalization (n=56) |
||
One day before surgery |
28 |
50 |
The day of surgery |
28 |
50 |
Exit |
||
After one day |
5 |
8,9 |
After two days |
33 |
58,9 |
After three days |
18 |
32,2 |
Table 2: Cancer and the preoperative care characteristics
The different waiting times of the surgical pathway of women with breast cancer
The global waiting time to first treatment (surgery) which extends from the time of radiological diagnosis to the time of surgery was 78,5% ±SD days. The global waiting time of access to surgery, starting from the date of the decision to treat after the multidisciplinary discussion to the surgery (day of the treatment) was 43,5% ± SD days. The different waiting times are presented in the Table 3.
| Time | Definition | Number (n) | Median [IIQ] (days) | [Min-Max] |
|---|---|---|---|---|
| The first intermediate time (the waiting time to access to diagnosis) | Between the radiological diagnosis and the pathological diagnosis (Anatomopathological results). | 61 | 8 [4,5-20] | [0-206] |
| The second intermediate time (the waiting time to access to first treatment: surgery) | Between the pathological diagnosis (biopsy) of the breast cancer and the start of the treatment. | 47 | 66 [50-90] | [20-225] |
| The global waiting time to first treatment (surgery) | Between the radiological diagnosis and the start of the surgery. | 56 | 78,5 [55,5-113,25] | [29-252] |
| The appointment waiting time | Is the time between the day which the patient is presented to make an appointment and the date of the first consultation | 42 | 15 [6-28] | [0-90] |
| The waiting time to diagnosis | Is the time between the first consultation and the last consultation before the multidisciplinary discussion. | 77 | 9 [0-28,5] | [0-180] |
| The waiting time to the multidisciplinary discussion | Is the time between the last consultation and the multidisciplinary discussion date | 77 | 4 [1-6] | [0-12] |
| The information period | Is the period between the multidisciplinary discussion and the date of the receipt of the information by the patient | 67 | 10 | [0-80] |
| The waiting time to the pre-anesthesic consultation | Is the time between the receipt of the information and the pre-anesthesic consultation. | 64 | 5 [2-9,75] | [0-41] |
| The time to surgery | Is the time between the pre-anesthesic consultation and the surgery. | 64 | 6 [4-8,75] | [0-69] |
| The global time of access to surgery | Is a global time between the multidisciplinary discussion (date of the decision to treat) and surgery (treatment). | 56 | 43,5 [40-54,75] | [5-91] |
Table 3: Study of the waiting times of the care pathway of women with breast cance.
Discussion
Being diagnosed with breast cancer can lower a patient’s quality of life. A long waiting time for surgery will certainly cause stress and anxiety (Rapoport Y, et al., 1993) and can deepen the spread of the tumor. There is no fixed waiting time from diagnosis to surgery, but it’s recommended once the diagnosis is made to start the surgery as quickly as possible. However, it’s important to note that international comparisons must be interpreted with caution, because of the different definitions of waiting times before treatment, the methodologies used and above all because of the complexity and diversity of the management strategies in each healthcare system (Limam M, et al., 2016).
In our study the sample consisted of 77 women. Ten waiting times have been calculated. The most important: The Global time to first treatment (surgical treatment) was 78.5 days with an Interquartile range (IIQ) of [55.5-113.25 days]. The information period was 10 days with an IIQ of [3-19 days] and the global time of access to surgery was 43.5 days with an IIQ of [40-54.75].
Estimating waiting times to surgery can help countries follow the efficacy of their healthcare system for cancer patients, and to increase awareness of effective and timely care. The first intermediate time (the waiting time to access to the diagnosis), varies between 13 days according to the studies of Limam M, et al., 2016, Poucel G, et al., 2013, Rayson D, et al., 2004 and 22 days in the study of Revaux A, et al., 2014. According to international recommendations this period should not exceed 28 days. Compared to previous studies, the 8-day timeframe found in our study is the shortest. The second intermediate time (the waiting time to access to first treatment (surgery), was unfortunately the highest. In literature, it was around 12 days in the study of Revaux A,et al. , 2014, 22.9 days in the study of Poucel G, , 2013 and 29 days in the study of Alberta in Canada (Li X,et al., 2013). Regarding the global waiting time to surgery which is surgery, according to the literature, it varied between 10 days to 52 days (MoliniéF,et al., 2013;Limam M, , 2016; Mayo NE, et al.,2001). According to the Na-tional Institute of Health and Clinical Excellence (NICE) (National Institute for Health, 2001), the British Association of Oncology (BASO) (British Association of Surgical Oncologists, 2005) and the National Health Service Cancer Plan 2000 (Department of Health, 2000), the HAS (High Authority of Health) recommended maximum waiting time is 4 weeks and indeed 90% of the patients were able to access to treatment within this timeframe. In our study, only one patient had surgery within the first month after diagnosis.
To avoid inconsistent patients care management, it is important to analyze the patient care pathway and create a structured process especially with the increasing complexity of breast cancer treatment. The main goals of establishing a care pathway consist of improving the quality of care, reducing risks and monitoring patient waiting times before surgical treatment (de Bleser L,et al., 2006). Moreover, to be effective, the healthcare system must measure and evaluate how long it takes for the patient to get through all the steps needed to finalize her treatment in order to ensure the best quality services (Li X,et al. , 2013). In addi-tion, waiting times evaluation is not just a direct reflection of internal managing systems but also of continuity of care and coordination between several care providers (Rutqvist LE, 2006). Nonetheless, the continuous growing complexity of the patient care trajectory reveals more and more inequalities to care access. Several waiting periods are calculated considering the patient care trajectory and the most important ones, which can cause problems and directly influence delays, are: the appointment time. It starts from the first patient’s contact with the healthcare system to the first consultation. Appointment waiting time represents “the system delay” and should be distinguished from the “patient delay” which starts from the day of symptoms onset to the first patient contact with the healthcare system.
There are no standards defining the optimal appointment time. In fact, this time varies a lot in the literature. The National Health Service Cancer Plan recommends a maximum of two weeks for the first consultation for 93% of cases (Pourcel G, et al., 2013). The European Society of Surgical Oncology (ESSO) recommends that 80% of urgent cases referred must be seen by a specialist within 5 days, and 70% of non-urgent cases must be seen within 15 days (Blichert-Toft M, et al., 1997). The British Association of Surgical Oncology (BASO) (British Association of Surgical Oncologists, 2005) recommends for 90% of patients to not exceed two weeks for urgent cases and three weeks if the situation is considered less urgent. Despite the fact that 75 out of the 77 women in our study have had a mammogram before the first consultation which was suspicious in 92.2%, only 52.3% of them had an appointment in less than two weeks. This long waiting time for the first appointment with a specialist for breast cancer patients compared to the literature, could be explained by several factors. For example, the healthcare professionals dealing with appointment schedules are not sufficiently qualified to estimate the urgency and severity of the situation. Also, the general practitioner or the midwife who refers the patient, do not emphasize enough in their referral letter on the suspicious diagnosis of breast cancer.
The second important time is the waiting time to diagnosis between the first and the last consultation (diagnosis formulation). This time frame calculated for all our patients (N=77) has a median of 9 days with an Interquartile range of [0-28.5 days].
In reference to this time, NHS England is working towards a new target called the Faster Diagnosis Standard (FDS). The objective is that the patient should not wait for more than 28 days from referral to finding out whether he or she has cancer. This process is meant to ensure that patients do not have to wait too long to find out their diagnosis (National Institute for Health, 2001; England NH and Improvement NH, 2018). Delays in breast cancer care, and waiting for definitive diagnosis after an abnormal screening mammogram is an intense and often agonizing experience for women involved and for their families (Thorne SE, et al., 1999). In our study, 40,3% of cases have had an immediate decision, which means that in the first consultation the diagnosis has been formulated, whereas 59,7% required two consultation or more. Moreover, the specialist may need to do a variety of investigations in order to obtain the final diagnosis or to eliminate differential diagnoses in case the patient has not done the mammogram, but comparing to the first preoperative quality indicator related to clinical pathways and care access in breast cancer (proportion of women with breast cancer who pre-operatively underwent mammography, ultrasound and physical examination) who required a minimum standard of 90% and a target of 95%, our result is satisfactory (Biganzoli L, et al., 2017). Also we found that 79.2% of the patients with suspected radiological diagnosis pre-operatively underwent biopsy to confirm the diagnosis.
With regard to the multidisciplinary discussion, it is one of the internal organization criteria of the service that brings together qualified health professionals from different disciplines to make a decision for the definitive diagnosis based on the radiological and the anatomopathological results. The National Institute for Clinical Excellence recommends multidisciplinary discussion at some point during the care process. Files examination during a multidisciplinary committee is in itself a guarantee not only of the best treatment option chosen but also of the quality of care (National Institute for Health, 2001). The management of breast cancer by a multidisciplinary team seems to be associated with a significant improvement in the survival rate (Guller U, et al., 2005). In our study, this time (the waiting time to the multidisciplinary discussion) was calculated for all the women. Due to the increasing complexity of breast cancer patient management and the cancer care paradigm change from a disease-focused management to a patient centered approach, having multidisciplinary staff become an key factor in quality indicators (Borras JM, et al., 2014). Besides, according to Héquet D, et al. discussing breast cancer cases in multidisciplinary meetings can lead to changes in surgical management recommendations in 12 to 52% of cases (Héquet D, et al., 2017). In the current study, most women (80.5%) had to wait between 1 to 7 days for their files to be discussed during the multidisciplinary meeting, only 9.1% of files were discussed the same day the diagnosis was made. In our study, we have considered the time between the multidisciplinary discussion (in which a final decision was made regarding the surgical procedure) and the date the patient was informed of this decision. Our results highlighted a dysfunction in this process in reference to when, how and by whom the patients were informed. In fact, patients had to contact themselves the department to obtain any information relative to their appointment and if the patient forgets to contact the service, she will miss her surgical appointment. In our department, a nurse was charged to inform the patient of the date of the operation, without any extra information about the type of surgery. International recommendations suggest that the attending physician should announce the final diagnosis after having discussed the file with a multidisciplinary team, in a special announcement and information consultation, in which the surgeon takes time to answer the patient's questions (National Institute for Health, 2001). Actually, proper diagnoses announcement and clear and simplified information decrease significantly psychological morbidity by reducing anxiety and complains, and increasing treatment adherence (National Institute for Health, 2001). Considering the patient’s information process in our setting, we suggest that the nurse should play a crucial role in facilitating the patient’s journey through the surgical pathway, like Saint-Augustinus Hospital experience in Belgium who introduced in 2005 a specialized nurse to facilitate the patient’s journey through the multidisciplinary track and to be a gate keeper of the clinical pathway is an example to follow (Plotogea A, et al., 2013). In our study, we have also considered waiting times from diagnosis to surgery (the global waiting time of access to surgery). This is a global time between the multidisciplinary discussion (date of the decision to treat) and surgery (treatment) which give us an idea about delays to undergo the surgery. Although, there are no standard guidelines defining the appropriate time from diagnosis to surgery for patient with breast cancer, it is obviously recommended to accelerate treatment once the diagnosis is made. The median of this time was 43.5 days with an Interquartile range of [40-54.75 days]. Almost half of the women (48.1%) needed at least one to two months to undergo surgery. Only eight women (10.4%) had to wait for less than one month which is higher than reported in several studies. Studies in France reported this waiting time to be between 13.5 and 22.9 days (Pourcel G, et al., 2013; Revaux A, et al., 2014). It was around 17 days in Canada (Plotogea A, et al., 2013) and 30 days in the United States (Plotogea A, et al., 2013). Cancer Care Ontario recommends a maximum period of 28 days between the decision to treat and surgery for invasive breast cancer (Bleicher RJ, et al., 2012). The UK National Health Service (NHS) recommendations pointed out that time between diagnosis and first treatment should not exceed 31 days (Vujovic O,et al, , 2009). Based on “Guidelines for the management of symptomatic Breast cancer”, this waiting time between the decision to treat and the surgery should not exceed two weeks (British Association of Surgical Oncologists, 2005).
The WHO (World Health Organization, 2017) defines quality of care as "the extent to which health care services provided to individuals and patient populations improve desired health outcomes. In order to achieve this, health care must be safe, effective, timely, efficient, equitable and people-centered". The time to care, in its various components,is an important quality indicator and a crucial element that can condition patient’s prognosis, particularly those with breast cancer. Reducing these delays in providing care must be integrated into a continuous quality improvement approach where decision-making is based on evidence-based data to take appropriate corrective actions. Surgery spans the entire cancer continuum, as it is often required for diagnosis, staging, treatment or palliation. It is usually one of the first contact points of the patient with the cancer care system and 80% of cancer patients can expect to undergo surgical intervention. A well organized pathway can improve quality of care and significantly reduce waiting time.
Highlights
To our knowledge this is the first study in Tunisia to investigate step by step the surgical pathway of women with breast cancer.
This is also the first study to analyze the global and the different waiting times to surgical treatment of women with breast cancer at the same time, making it possible to identify any malfunctions that occur during this process and to investigate the causes.
We tried to set up a quality indicator to be used by the decision makers as a key element in the quality and continuity of care. It is also a performance indicator of the healthcare system and a tracer of inequalities in access to healthcare
In addition, to this moment there are no national healthcare society’s recommendations about this quality indicator. The data collected in this study allow us to compare with other societies guidelines if the study is conducted elsewhere. It will also help us following the evolution of this indicator after implementing corrective actions
A good control of waiting times during the treatment process and avoiding delays in breast cancer treatment is obviously crucial to ensure the best possible outcomes for patients diagnosed with breast cancer.
Conclusion
Despite limitations consisting mainly in the small sample size and there is often missing data with regard to the dates (dates of taking appointment, dates of consultations, dates of explorations, date of onset of symptoms and dates of assumption of responsibility) which makes it difficult to calculate certain deadlines, moreover some dates were hardly documented despite the notion of achievement of the diagnostic or therapeutic act. Our prospective study enabled a deep evaluation of practice, the objective was to identify dysfunctional processes and plan corrective measures to ensure the best possible care for patients diagnosed with breast cancer. Further studies are needed to evaluate the impact of the different delays to treatment on patient’s survival and treatment outcome and the impact of some improvement axes to reduce delays and subsequently improve survival.
Declarations
Ethics approval and consent to participate
• This protocol was approved by the medical ethics committees of Farhat Hached university hospital.
• A verbal consent and agreement from the head of the center was obtained.
• Also a clear, informed and oral consent was taken by the patients.
• Anonymity and confidentiality of data have been ensured.
• Data collection was carried out by a single investigator.
• The collection of the data was prospective to guarantee the completeness of the data collection and to avoid the missing data.
Availability of data and materials
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
Place of study
The gynecology obstetric department located in the Maternity and Neonatal Center of Sousse offers a very large volume of activities for the governorate of Sousse and others governorates. In 2017, this service provided 21,072 hospitalizations with 9,103 operative activities including 4379 gynecological surgeries. Concerning the breast cancer: the total number in 2017 was 676 (28.41% of surgical procedures in gynecology) including 279 cases of conservative treatments and 397 of radical treatment.
The data were collected using an anonymous data collection sheet developed for the purpose of this study. This sheet was designed to follow the surgical pathway of women diagnosed with breast cancer using the method of process which describe in details all the stages of the process undergoing by the patient and calculate at the same time the different waiting times.
In order to obtain the different data and dates for each patient, different document have been consulted (medical files, department registers, etc.) as well as interviews with healthcare professionals and administrative staffs involved in the process.
Authors’ contributions
This work was carried out in collaboration between all authors,
P. Ajmi Thouraya and P. Mtiraoui Ali: Designed the study, coordinated the study and manuscript editing.
P. Khairi Hedi: The guarantor of the integrity of the study and the final approval of the version.
Manel Limam: Definition of intellectual content, analysis and interpretation of data.
Sahli Jihene: Statistical analysis, analysis and interpretation of data.
Kahlaoui Meriam: Literature research, data acquisition, analysis and interpretation of data and wrote the first draft of the manuscript.
All authors read and approved the final manuscript.
Acknowledgements
To all the team of The Gynecology Obstetric Department Chu Farhat Hached Sousse and all the staff of the secretariat for their invaluable assistance during data collection and for their collaboration and invaluable help in carrying out this work.
References
- Torre LA, Bray F, Siegel RL, Ferlay J, Lortet‐Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015; 65(2): 87-108.
- WHO. Global Status Report on No Communicable Diseases 2010. Geneva: World Health Organization. 2010.
- WHO. Global Status Report on No Communicable Diseases 2018. Geneva: World Health Organization. 2018.
- Cherif A, Dhaouadi S, Osman M, Hsairi M. Breast Cancer burden in Tunisia: Situation in 2017 and projections by 2030. Eur J Public Health. 2019; 29(4): ckz186-232.
- Ministry of Health. Plan for the Fight Against Cancer in Tunisia 2015-2019. International Cancer Control Partnership. 2020.
- Landolsi A, Gahbiche S, Chaafii R, Chabchoub I, Leila BF, Mafram H. Causes of Delayed diagnosis of breast cancer in Tunisian women: Series of 160 patients at the Tunisian center. La Tunisie Medicale. 2010; 88(12): 894-897.
- Molinié F, Leux C, Delafosse P, Ayrault-Piault S, Arveux P, Woronoff AS, et al. Waiting time disparities in breast cancer diagnosis and treatment: A population-based study in France. Breast. 2013; 22(5): 810-816.
- Pourcel G, Ledesert B, Bousquet PJ, Ferrari C, Viguier J, Buzyn A. Waiting times for cancer care in four most frequent cancers in several French regions in 2011 and 2012. Bull Cancer. 2013; 100(12): 1237-1250.
- Revaux A, Laas E, Chopier J, Thomassin-Naggara I, Touboul E, Antoine M, et al. Delays in treatment of breast cancer: Experience of an expert center of the Assistance Publique-Hôpitaux de Paris (AP-HP). Gynecol Obstet Fertil Senol. 2014; 42(9): 585-590.
- Bleicher RJ, Ruth K, Sigurdson ER, Beck JR, Ross E, Wong YN, et al. Time to surgery and breast cancer survival in the United States. JAMA Oncol. 2016; 2(3): 330-339.
- Webber C, Whitehead M, Eisen A, Holloway CM, Groome PA. Breast cancer diagnosis and treatment wait times in specialized diagnostic units compared with usual care: A population-based study. Curr Oncol. 2020; 27(4): 377-385.
- Colleoni M, Bonetti M, Coates AS, Castiglione-Gertsch M, Gelber RD, Price K, et al. Early start of adjuvant chemotherapy may improve treatment outcome for premenopausal breast cancer patients with tumors not expressing estrogen receptors. J Clin Oncol. 2000; 18(3): 584.
- Shin DW, Cho J, Kim SY, Guallar E, Hwang SS, Cho B, et al. Delay to curative surgery greater than 12 weeks is associated with increased mortality in patients with colorectal and breast cancer but not lung or thyroid cancer. Ann Surg Oncol. 2013; 20(8): 2468-2476.
- Rapoport Y, Kreitler S, Chaitchik S, Algor R, Weissler K. Psychosocial problems in head-and-neck cancer patients and their change with time since diagnosis. Ann Oncol. 1993; 4(1): 69-73.
- Limam M, Ajmi T, Zedini C, Khelifi A, Mellouli M, El Ghardallou M, et al. Study of breast cancer treatment waiting times in Sousse, Tunisia. Sante Publique. 2016; 28 (3): 331-340.
- Rayson D, Chiasson D, Dewar R. Elapsed time from breast cancer detection to first adjuvant therapy in a Canadian province, 1999-2000. Can Med Assoc J. 2004; 170(6): 957-961.
- Li X, Scarfe A, King K, Fenton D, Butts C, Winget M. Timeliness of cancer care from diagnosis to treatment: A comparison between patients with breast, colon, rectal or lung cancer. Int J Qual Health Care. 2013; 25(2): 197-204.
- Mayo NE, Scott SC, Shen N, Hanley J, Goldberg MS, MacDonald N. Waiting time for breast cancer surgery in Quebec. Can Med Assoc J. 2001; 164(8): 1133-1138.
- National Institute for Health. National Institute for Health and Care Excellence: Clinical Guidelines. National Institute for Health. 2001.
- British Association of Surgical Oncologists. Guidelines for the Management of Symptomatic Breast Disease. British Association of Surgical Oncologists. 2005.
- Department of Health. The NHS Cancer Plan. National Institute for Health. 2000.
- de Bleser L, Dep reitere R, de Waele K. Defining pathways. J Nurs Manag. 2006; 14(7): 553-563.
- Rutqvist LE. Waiting times for cancer patients-a “slippery slope” in oncology. Acta Oncol Stockh Swed. 2006; 45(2): 121-123.
- Blichert-Toft M, Smola MG, Cataliotti L, O'Higgins N. Principles and guidelines for surgeons-management of symptomatic breast cancer. Eur J Surg Oncol. 1997; 23(2): 101-109.
- England NH. Improvement NH. Diagnosing Cancer Earlier and Faster. 2018.
- Thorne SE, Harris SR, Hislop TG, Vestrup JA. The experience of waiting for diagnosis after an abnormal mammogram. Breast J. 1999; 5(1): 42-51.
- Biganzoli L, Marotti L, Hart CD, Cataliotti L, Cutuli B, Kühn T, et al. Quality indicators in breast cancer care: An update from the EUSOMA working group. Eur J Cancer. 2017; 86: 59-81.
- Guller U, Safford S, Pietrobon R, Heberer M, Oertli D, Jain NB. High hospital volume is associated with better outcomes for breast cancer surgery: Analysis of 233,247 patients. World J Surg. 2005; 29(8): 994-999.
- Borras JM, Albreht T, Audisio R, Briers E, Casali P, Esperou H, et al. Policy statement on multidisciplinary cancer care. Eur J Cancer. 2014; 50(3): 475-480.
- Héquet D, Huchon C, Baffert S, Alran S, Reyal F, Nguyen T, et al. Preoperative clinical pathway of breast cancer patients: Determinants of compliance with EUSOMA quality indicators. Br J Cancer. 2017; 116(11): 1394-1401.
- Plotogea A, Chiarelli AM, Mirea L, Prummel MV, Chong N, Shumak RS, et al. Factors associated with wait times across the breast cancer treatment pathway in Ontario. Springerplus. 2013; 2(1): 1-9.
- Bleicher RJ, Ruth K, Sigurdson ER, Ross E, Wong YN, Patel SA, et al. Preoperative delays in the US Medicare population with breast cancer. J Clin Oncol. 2012; 30(36): 4485.
- Vujovic O, Yu E, Cherian A, Perera F, Dar AR, Stitt L, et al. Effect of interval to definitive breast surgery on clinical presentation and survival in early-stage invasive breast cancer. Int J Radiat Oncol Biol Phys. 2009; 75(3): 771-774.
- World Health Organization. What is quality of care and why is it important. World Health Organization. 2017.
Author Info
Kahlaoui Meriam1*, Limam Manel1, Sahli Jihene1, Khairi Hédi2, Mtiraoui Ali1 and Ajmi Thouraya12Department of Gynecology and Obstetrics, University of Sousse, Sousse, Tunisia
Received: 13-Jul-2021 Accepted: 27-Jul-2021 Published: 03-Aug-2021
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






