Research Article - (2023) Volume 14, Issue 1
Effectiveness of Ketac Nano Restoration in Class II Cavities in Primary Molars: A Randomized Controlled Clinical Trial
Amr H Ali1*, Ahmed A Mohamed2 and Dalia M Talaat1Abstract
Introduction: Nanofilled glass ionomer cement emerged as a new generation of dental materials, which mineralizes gradually into fluorapatite to improve the compressive strength and wear resistance of class II restorations in primary molars. The purpose of this study was to evaluate clinically the effectiveness of glass carbomer cement with surface coat as class II restorations in primary molars in comparison to both of Ketac N 100 glass ionomer cement with surface coat and conventional glass ionomer cement with surface coat (Equia Fill).
Materials and methods: This randomized controlled clinical trial included a sample of 117 children were selected with an age range of 4-7 years, having class II carious primary molars scoring 3, 4 or 5 (ICDAS II). They were randomly equally allocated into three groups according to the restorative material used- Group I (test): Teeth were restored with glass carbomer cement, Group II (test): Teeth were restored with Ketac N 100 glass ionomer cement and Group III (control): Teeth were restored with (Equia Fill). Clinical evaluation was performed at baseline, 6 and 12 months.
Results: Nano filled GICs (Ketac N and glass carbomer cement) showed significant higher retention rate and durability than Equia fill GIC at three examination times (baseline, 6 and 12 months) P<0.0001. Regarding the effect of the restorations on periodontal health there were statistically significant difference between the three study groups at baseline and 6 months P<0.0001. No statistically significant differences were found between three study groups at 12 months P=0.02.
Conclusion: Nanofilled GICs were more effective in restoring class II cavities in primary molars as well as having better consequential effect on the periodontal health compared to the conventional GICs.
Keywords
Glass carbomer cement, Fluorapatite, Conventional glass ionomer cement, Nano fillers
Introduction
Dental caries is the most frequent chronic childhood disease worldwide (Ozdemir D, 2013). Untreated caries may affect seriously the quality of children’s life because of pain and acute or chronic infections which may compromise eating and sleeping leading to learning disorders (Agaku IT, et al., 2015). Further more, primary teeth when left untreated, lead to detrimental impact on the permanent dentition due to loss in the space available in the dental arch and consequently leading to crowding and malocclusion (Skeie MS, et al., 2006) or developmental defects of the permanent successor teeth (Broadbent JM, et al., 2005). Therefore, maintaining the integrity of dental arch in the primary dentition is considered crucial for establishing normal occlusion and function in the permanent dentition (Broadbent JM, et al., 2005; Walsh T, et al., 2010; AAPD, 2008).
Along the way to preserve tooth structure and for the application of minimal intervention concept, micro-conservative dentistry has emerged in which a minimum of tooth structure is removed (Beltrán-Aguilar ED, et al., 2015). Following this concept slot preparation advocated by Wilson and Mclean (Murdoch-Kinch CA and McLean ME, 2013), involves the removal of the marginal ridge but do not include all the occlusal pits and fissures.
The innovation generated along the way with restorative materials for restoring primary molars led to the development of glass ionomers to replace the traditional silver amalgam for better retention in the conservative cavity preparations (Frencken JE, et al., 2012). Conventional Glass Ionomer Cement (GIC) has the ability to chemically bond to tooth structure and release fluoride, with additional benefits of biocompatibility, antibacterial effects (Ensaff H, et al., 2001; Donly K, 2002). However, it’s prolonged setting time compromise its physical and mechanical properties especially in restoring class II cavities in primary teeth. Therefore, in an attempt to improve its properties, a variety of modifiers have been added to its matrix (Palin WM and Fleming GJ, 2003).
A promising new technology (Nanotechnology) is applied in the dental field. Using this technology, glass carbomer cement and Ketac N have been introduced as GIC-based restorative materials, with claims of improved physical and mechanical characteristics (Yap AU, et al., 2003; Cehreli SB, et al., 2013; Gorseta K, et al., 2014; van Duinen RN, et al., 2004; Hassan A, et al., 2016; Nassar AM, et al., 2014).
Considering the few published clinical data, on newly developed nanosized glass ionomer cements (Yap AU, et al., 2013; Cehreli SB, et al., 2013; Gorseta K, et al., 2014; van Duinen RN, et al., 2004; Hassan A, et al., 2016; Nassar AM, et al., 2014). The present study was initiated to assess the clinical performance of these materials as well as the provision of valuable insights into their enhanced physical and mechanical properties, when used in class II restorations in primary teeth. The null hypothesis of the current research was expecting no differences between the glass carbomer cement, ketac N glass ionomer and the conventional glass ionomer cement in clinical assessment.
Materials and Methods
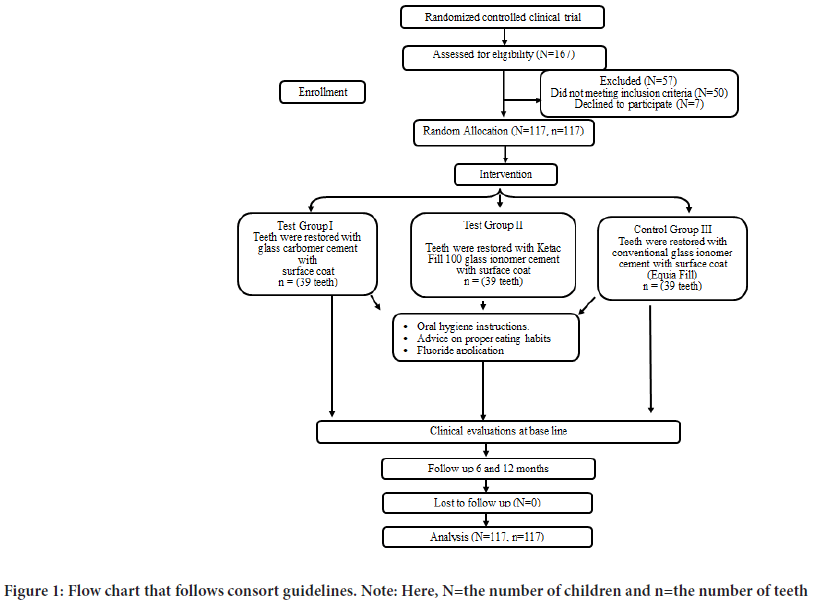
This study was a randomized controlled clinical trial, with equal allocation ratio 1:1:1. It was setup and reported according to the CONSORT guidelines (Viera AJ and Bangdiwala SI, 2007) (Figure 1).
Figure 1: Flow chart that follows consort guidelines. Note: Here, N=the number of children and n=the number of teeth
The study was approved from the Research Ethics Committee, Faculty of Dentistry, Alexandria University, Alexandria, Egypt, and registered at the National Institutes of Health. Healthy high-caries risk children with active class II cavities in primary molars scored 3, 4 or 5 according to the International Caries Detection and Assessment System (ICDAS II scoring system) without involvement of the buccal and lingual walls. They were between 4 and 7 years old. The participants were recruited from the out patient clinic, Pediatric Dentistry and Dental Public Health Department, Faculty of Dentistry, Alexandria University.
Sample size estimation
Sample size was estimated based on the following assumptions-Alpha error=5%, study power=80%, confidence level=95%. A power of 80% and a significance level of P value ≤ 0.05 (Gorseta K, et al., 2016), Sample size was based on Rosner’s method (HHU, 2019; Gunda S and Varma N, 2019) was calculated by G power 3.0.10. After 12 months, the overall success rates were 56% for glass carbomer cement and 86% for conventional GIC (Equia Fill) based on previous study (de França CM, et al., 2018), sample size was calculated to be 35 children, and this was increased to 39 to make up of cases lost to follow up. The total sample size=number of groups × number per group=3 × 39=117 child.
Patient’s recruitment
Out of 167 screened children who attended the outpatient clinic of Pediatric Dentistry and Dental Public Health Department, Faculty of Dentistry, Alexandria University, 117 children who met the inclusion criteria were enrolled in the clinical trial after informing their parents about the study protocol and signing their informed consent.
Oral hygiene instructions
All participants received oral hygiene instructions and dietary guidance in each visit throughout the entire study period. Parents were instructed to refrain from brushing their children’s teeth (Nassar AM, et al., 2014).
Randomization technique and allocation concealment
Random allocation of each participant to Group I glass carbomer cement and Group II Ketac N100 glass ionomer cement (test groups) and Group III conventional glass ionomer cement (positive control) was performed by atrial independent individual using computerized method (www.radomizer.org) and the allocation ratio was intended to be equal. Allocation was in equal blocks to ensure that the study groups had equal number of children.
Each child included in this study was given serial number that was used in allocation. A duplicate of this number was kept in an opaque envelope indicating to which group the patient belongs. An independent person who was assigned the role of opening each envelop only at the time of intervention; so that the group to which the child is allocated was concealed from the investigator (Ekstrand KR, et al., 2007).
Blinding
Blinding of examiners was impossible to be done during intervention and follow up due to different natures of the materials. However, for patients and statistical analysis, the statistician and patients were not known to which group the data belongs (double blinding).
Examiner reliability
The main researcher was trained for assessing the lesion activity by (IC- DAS II scoring system) and Ryge Criteria for direct clinical evaluation of restoration (Hickel R, et al., 2007), The evaluation systems used were Modified Papillary Bleeding Index and modified gingival index (Hickel R, et al., 2007; Moszner N and Klapdohr S, 2004), and a pilot study was carried out on 20 percent of the sample that was not included in the study, to calibrate the researcher for the aforementioned assessments. Intraexaminer reproducibility was assessed by calculating Intraclass Correlation Coefficients (ICCs) and Cohen’s kappa coefficient (K) for the (ICDAS II), Ryge Criteria, (MPBI Scale) and modified gingival index respectively. Intraexaminer reproducibility revealed excellent ICCs (0.92) and K (0.81).
Sample grouping
All samples were randomly assigned into 3 groups (n=39/each) according to the restorative material tested.
Test group I: Teeth were restored with glass carbomer cement with surface coat.
Test group II: Teeth were restored with Ketac N 100.
Control group: Teeth were restored with conventional glass ionomer cement with surface coat (Equia Fill).
Intervention
Topical anesthesia was applied then infiltration or nerve block anesthesia was given. The selected tooth was isolated with rubber dam and the tooth surface was cleaned with wet cotton pellet to remove debris and plaque. A gingival wedge was placed prior to initiating cavity preparation. Class II slot preparation with occlusal lock was performed where all infected tissue was removed from the surrounding walls and the enamel-dentin junction using #330 bur with water cooling (Gunda S and Varma N, 2019).
After the cavity preparation, a metallic matrix was cut, burnished, positioned and stabilized by a wooden wedge to define the proximal contour of the restoration.
For all the prepared cavities, cavity conditioner was applied to enamel and dentin surfaces and left undisturbed for 10 seconds, then the cavity was rinsed with water for 10 seconds and was gently air-dried for 5 seconds (Gunda S and Varma N, 2019). Teeth of all groups were restored according to manufactures instructions.
Teeth restoration
For test group I: Glass carbomer cement capsule was mixed by the amalgamator for 10-15 seconds; placed into the cavity, and light cured for 10 seconds (de França CM, et al., 2018).
For test group II: Ketac N 100 glass ionomer cement was mixed by the amalgamator for 10 seconds; placed into the cavity and light cured for 10 seconds (de França CM, et al., 2018).
For control group: Conventional glass ionomer cement was mixed by the amalgamator for 10 seconds; applied into the cavity and light cured for 10 seconds (de França CM, et al., 2018).
The restorations of all teeth included in the study were finished and polished using rubber cups (23). Teeth in test group I and control group were coated with surface coat and light cured for 10 seconds by using LED light curing system (de França CM, et al., 2018).
After completion of the restorative procedures, all teeth in the three groups were evaluated at base line, 6 and 12 months. Debris and plaque on the tooth surfaces were removed before evaluation using a wet cotton pellet.
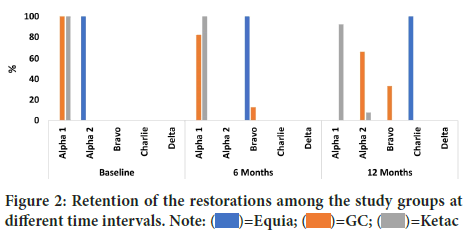
Evaluation of retention rate
Clinical evaluation was performed through visual inspection at baseline, 6 and 12 months follow up, using Ryge Criteria for direct clinical evaluation of restoration. The restorations were evaluated by taking different scores from Alpha 1 (clinically excellent), Alpha 2 (clinically good), Bravo (clinically sufficient with few defects), Charlie (restoration partially missed), Delta (restoration is totally missed) according to the degree of restoration lost (Figure 2) (Hickel R, et al., 2007).
Figure 2: Retention of the restorations among the study groups at different time intervals. Note:  =Equia;
=Equia;  =GC;
=GC;  =Ketac
=Ketac
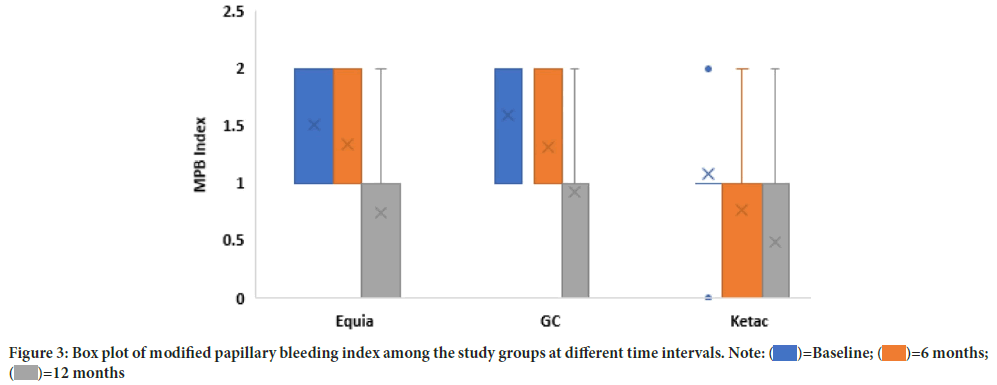
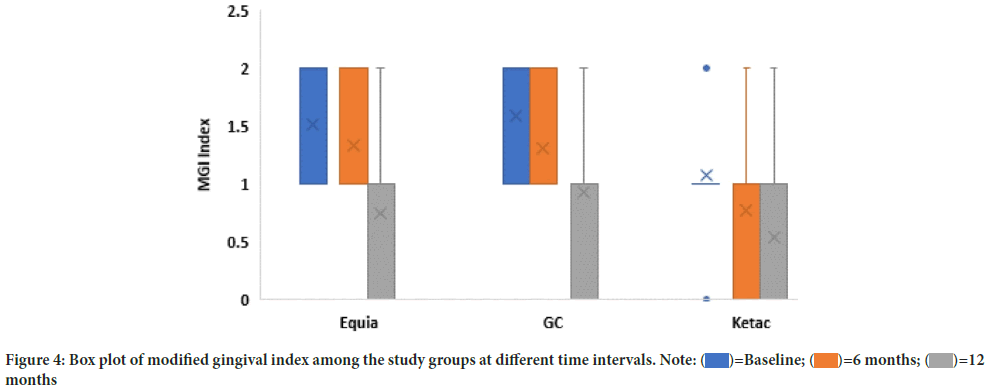
Effect of the restoration on the periodontal health
Clinical evaluation was performed at baseline, 6 and 12 months follow up, using the criteria of Modified Papillary Bleeding Index (MPBI) and Modified Gingival Index (MGI). The restorations were evaluated by taking different scores for (MPBI) evaluation scores from 0 (no bleeding within 30 secs of probing), 1 (bleeding between 3 to 30 secs of probing), 2(bleeding within 2 secs of probing), 3 (bleeding immediately upon probing) and for (MGI) evaluation scores 0 (absence of inflammation) ,1 (mild inflammation or slight changed in color or texture), 2 (mild inflammation in all gingival margins or papillary) , 3 (moderate inflammation ),4 (severe inflammation) (Hickel R, et al., 2007; Moszner N and Klapdohr S, 2004).
Statistical analysis
Data were analyzed using IBM SPSS (Statistical Package for Social Science) statistical software (version 25). The collective quantitative data was tested for normality, which was confirmed using Shapiro Wilk test. Descriptive statistics were summarized using mean and standard deviation (SD). Independent t test was used for intergroup comparisons. Repeated measures ANOVA with post hoc Bonferroni test for intragroup was used to compare retention rate and effect of the restoration on the periodontal health among the groups, with a P value ≤ 0.05.
Results
At baseline, 167 children (mean age equals 5.6 ± 0.80 SD) with a total of 167 class II cavities in primary molars were assessed for eligibility, 57 were excluded, and 117 children (65 males, 52 females) with 117 class II cavities were included in the study. All participants received the allocated intervention and no one has been lost during the different follow-up periods.
Regarding the retention of the restorations, at baseline comparing the three study groups, teeth restored with glass carbomer and ketac N GICs showed 100% alpha 1 scores while teeth restored with conventional GIC Equia Fill showed 100% alpha 2 scores with a statistically significant difference between the three study groups P<0.0001.
At 6 months follow up, teeth restored with glass carbomer cement showed 82.1% alpha 1 scores, those with Ketac N GIC showed 100% alpha 1 scores while teeth restored with conventional GIC Equia Fill showed 100% Bravo scores with statistically significant difference between the three study groups P<0.0001. After 12 months follow up, teeth restored with glass carbomer cement showed 66.7% alpha 2 scores, teeth restored with Ketac N GIC showed 92.3% alpha 1 scores while teeth restored with conventional Equia Fill showed 100% Charlie scores with statistically significant differences between the three study groups P<0.0001 (Table 1).
| Equia (n=39) | GC (n=39) | Ketac (n=39) | Test (p value) | ||
|---|---|---|---|---|---|
| n (%) | |||||
| Baseline | Alpha 1 | 0 (0%) | 39 (100%) | 39 (100%) | 116 (<0.0001*) |
| Alpha 2 | 39 (100%) | 0 (0%) | 0 (0%) | ||
| Bravo | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Charlie | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Delta | 0 (0%) | 0 (0%) | 0 (0%) | ||
| 6 Months | Alpha 1 | 0 (0%) | 32 (82.1%) | 39 (100%) | 101.583 (<0.0001*) |
| Alpha 2 | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Bravo | 39 (100%) | 5 (12.8%) | 0 (0%) | ||
| Charlie | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Delta | 0 (0%) | 0 (0%) | 0 (0%) | ||
| 12 Months | Alpha 1 | 0 (0%) | 0 (0%) | 36 (92.3%) | 109.607 (<0.0001*) |
| Alpha 2 | 0 (0%) | 26 (66.7%) | 3 (7.7%) | ||
| Bravo | 0 (0%) | 13 (33.3%) | 0 (0%) | ||
| Charlie | 39 (100%) | 0 (0%) | 0 (0%) | ||
| Delta | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Test (p-value) | 78 (<0.0001*) | 72.066 (<0.0001*) | 6 (0.050*) | ||
| Post hoc test | P1<0.0001*, P2<0.0001*, P3<0.0001* |
P1=1.00, P2<0.0001*, P3<0.0001* |
P1=1.00, P2=1.00, P3=1.00 |
||
Note: *Statistically significant difference at p value<0.05
P1: Comparison between baseline and 6 months; P2: Comparison between baseline and 12 months; P3: Comparison between 6 months and 12 months
Table 1: Retention of the restorations among the study groups at different examination times
For within group comparisons, teeth restored with glass carbomer cement at baseline, all teeth showed 100% alpha 1 scores, at 6 months follow up teeth showed 82.1% alpha 1 scores and 12.8% Bravo scores while at 12 months follow up 66.7% showed alpha 2 scores and 33.3% Bravo scores with statistically significant differences P<0.0001.While,teeth restored with ketac N GIC at baseline, showed 100% alpha 1 scores, at 6 months showed 100% alpha 1 scores and at 12 months showed 92.3% alpha 1 scores with no statistically significant differences P=0.050. Regarding the conventional GIC Equia Fill, at baseline all teeth restored showed 100% alpha 1 scores, at 6 months 100% showed Bravo scores and at 12 months 100% showed Charlie scores with statistically significant differences P<0.0001 (Table 2).
| FDI Criteria (Modified papillary bleeding index) | Equia (n=39) | GC (n=39) | Ketac (n=39) | Test (p value) | |
|---|---|---|---|---|---|
| Baseline | Mean (SD) | 1.51 (0.51) | 1.59 (0.50) | 1.08 (0.58) | 16.659 (<0.0001*) |
| Median (IQR) | 2.00 (1.0) | 2.00 (1.0) | 1.00 (0.0) | ||
| Min-Max | 1.0-2.0 | 1.0-2.0 | 0.0-2.0 | ||
| 6 Months | Mean (SD) | 1.33 (0.48) | 1.31 (0.47) | 0.77 (0.54) | 24.237 (<0.0001*) |
| Median (IQR) | 1.00 (1.0) | 1.00 (1.0) | 1.00 (1.0) | ||
| Min-Max | 1.0-2.0 | 1.0-2.0 | 0.0-2.0 | ||
| 12 Months | Mean (SD) | 0.74 (0.78) | 0.92 (0.66) | 0.49 (0.60) | 7.811 (0.020*) |
| Median (IQR) | 1.00 (1.0) | 1.00 (1.0) | 0.00 (1.0) | ||
| Min-Max | 0.0-2.0 | 0.0-2.0 | 0.0-2.0 | ||
| Test (p value) | 30.868 (<0.0001*) |
25.31 (<0.0001*) |
17.083 (<0.0001*) |
||
| Post hoc test | P1=1.00 P2<0.0001* P3=0.001* |
P1=0.379 P2=0.001* P3=0.082 |
P1=0.210 P2=0.002* P3=0.302 |
||
| FDI Criteria (Modified gingival index) | |||||
| Baseline | Mean (SD) | 1.51 (0.51) | 1.59 (0.49) | 1.08 (0.58) | 16.659 |
| Median (IQR) | 2.00 (1.0) | 2.00 (1.0) | 1.00 (0.0) | (<0.0001*) | |
| Min- Max | 1.0-2.0 | 1.0-2.0 | 0.0-2.0 | ||
| 6 Months | Mean (SD) | 1.33 (0.48) | 1.31 (0.47) | 0.77 (0.54) | 24.237 |
| Median (IQR) | 1.00 (1.0) | 1.00 (1.0) | 1.00 (1.0) | (<0.0001*) | |
| Min- Max | 1.0-2.0 | 1.0-2.0 | 0.0-2.0 | ||
| 12 Months | Mean (SD) | 0.74 (0.78) | 0.92 (0.66) | 0.54 (0.60) | 6.014 |
| Median (IQR) | 1.00 (1.0) | 1.00 (1.0) | 0.00 (1.0) | (0.049*) | |
| Min- Max | 0.0-2.0 | 0.0-2.0 | 0.0-2.0 | ||
| Test (p value) |
30.868 (<0.0001*) |
25.31 (<0.0001*) |
17.083 (<0.0001*) | ||
| Post hoc test | P1=1.00 P2<0.0001* P3=0.001* |
P1=0.379, P2=0.001* P3=0.082 |
P1=0.210 P2=0.002* P3=0.302 |
||
Note: *Statistically significant difference at p value <0.05
Table 2: Comparison of modified papillary bleeding index and modified gingival index among the study groups at different examination times
By studying the effect of the restoration on the periodontal health, results of the present study revealed that the Modified Papillary Bleeding Index (MPBI) and modified gingival index (MGI) data showed statistically significant differences between the three study groups at baseline and 6 months follow up (P<0.0001, P<0.0001 respectively). Whereas, no statistically significant differences between the three study groups at 12 months follow up, regarding MPBI P=0.020 and MGI P=0.049.
Within group comparisons, regarding MPBI and MGI for teeth restored with glass carbomer GIC, Ketac N GIC and Equia Fill GIC results showed statistically significant differences at baseline, 6 and 12 months follow up ( P<0.0001, P<0.0001, P<0.0001 respectively) (Figures 3 and 4).
Figure 3: Box plot of modified papillary bleeding index among the study groups at different time intervals. Note:  =Baseline;
=Baseline;  =6 months;
=6 months;  =12 months
=12 months
Figure 4: Box plot of modified gingival index among the study groups at different time intervals. Note:  =Baseline;
=Baseline;  =6 months;
=6 months;  =12
months
=12
months
Repeated measures ANOVA analysis with post hoc Bonferroni test for intragroup revealed statistically significant differences for nanofilled GICs with P ≤ 0.05, regarding the retention rate and effect of the restoration on the periodontal health among the study groups.
Discussion
Results of the present study showed that both nanofilled GICs were more effective in restoring class II cavities in primary molars than conventional GIC. The differences between the three study groups necessitate rejection of the null hypothesis as the retention, sealing properties and effect on the periodontal health of nanofilled glass ionomer cements showed better results than conventional glass ionomer cement (Croll TP and Nicholson JW, 2002; Cehreli ZC and Gungor HC, 2008).
This study compared the clinical effectiveness of nanofilled GICs (glass carbomer, ketac N) to conventional GIC (Equia fill) in restoring class II cavities in primary molars. The inter group comparisons of the three study groups, showed a significantly higher retention rate of both ketac N and glass carbomer cement over the conventional glass ionomer with surface coat due to incorporations of nano particles which increases physical and mechanical properties of the restoration materials. However, this finding disagrees with the in-vitro study of Cehreli SB, et al., 2013 who found that there was no significant difference between coated glass carbomer and coated conventional GIC when restoring primary molars, so, the difference in the results may be attributed to the different nature of the study as evaluation the clinical performance of the restorations were affected by many factors such as forces of mastication, brushing and dietary habits and type of food intake.
Moreover, the results of the present study is in accordance with the data of Hassan A, et al., 2016 who evaluated the microleakage and marginal integrity of the newly developed glass carbomer cement with and without protective Surface Coating (SC) in primary molars. They found that, the surface coat when added to the glass carbomer cement yields less microleakage than the uncoated glass carbomer and conventional GIC and consequently might improve the longevity of the restoration which is one of the aims of the present study (Hassan A, et al., 2016).
In the coated restorations, the surface gloss used with the glass carbomer cement was more effective in its sealing ability as compared to the resinbased surface coating applied to the conventional GIC. Although, both restorative materials have common ingredients (e.g., glass), the manufacture does not provide detailed information regarding how the surface gloss acts, it is evident that its proprietary formulation provides better chemical interaction with the glass carbomer cement that enhances sealing properties (Derkson GD, et al., 1983; Feilzer AJ, et al., 1993; Aboush YE and Jenkins CB, 1987; Wilson AD, 1984; Mount GJ, 1982; Asmussen E, 1983).In the present study, ketac N showed significantly higher retention rate than conventional glass ionomer at baseline, 6 and 12 months follow up and when compared to glass carbomer cement at 12 months follow up only. This finding could be attributed to the composition of the ketac N glass ionomer cement and the manufacturer’s instructions which included using ketac N primer before application of the restoration to increase bond between tooth structure and restoration (Earl MS, et al., 1985; Rodrigues RCG, et al., 1995; Moshaverinia A, et al., 2011).
In the current study, within group comparison, teeth restored with glass carbomer cement and conventional GIC evaluated at baseline, 6 and 12 months follow up, results showed significant differences related to the mount of restoration lost along the different periods of examinations, more loss were scored in conventional GIC than glass carbomer cement while for teeth restored with Ketac N GIC, results showed no significant difference with lower rate of restoration loss along the different periods of examinations (Earl MS, et al., 1985; Rodrigues RCG, et al., 1995; Moshaverinia A, et al., 2011).
Regarding the effect of the restorations on the periodontal health that was assessed by evaluation systems of Modified Papillary Bleeding Index (MPBI) and Modified Gingival Index (MGI) (Watson T and Banerjee A, 1993). There were significant differences between the three study groups at baseline and 6 months follow up only with no significant differences between them at 12 months follow up. This may be due the long term effect of reinforcement of oral hygiene instructions and proper tooth brushing throughout the period of follow up and the consequent healing effect of the periodontium.
In the current study, within group comparison, teeth restored with glass carbomer cement, Ketac N GIC and conventional GIC evaluated at baseline, 6 and 12 months follow up, results showed significant differences that may be attributed to the enhanced periodontal health due to improvement in oral hygiene measures (Earl MS, et al., 1985; Rodrigues RCG, et al., 1995; Moshaverinia A, et al., 2011).
Conclusion
The overall results of the present study indicated that the nanofilled glass ionomer cement ketac N and glass carbomr cement with surface coat had better retention rate and proper marginal seal than conventional glass ionomer with surface coat. Moreover, the effect of the restorations on the periodontal health assessed by modified papillary index and modified gingival index showed better results.
The limitation of this clinical study is related to the short-term of the study (1-year follow-up) for the retention and sealing ability assessments. However, longer follow up periods would be interrupted by the physiological exfoliation of the teeth unless a younger age group would be used. Nevertheless, further trials with longer observation periods are still necessary to evaluate the esthetic, functional, and biological properties to document whether secondary caries which is regarded as the main reason for failure would develops in these restorations.
Based on the study’s results, the following conclusions can be made-
• Nano filled GICs were more effective than conventional GIC (Equia fill) in restoring class II cavities in primary molars when followed up for 12 months.
• Ketac N GIC showed better durability than glass carbomer cement after 12 months follow up in restoring class II cavities in primary molars.
• Nano filled GICs showed better effect on periodontal health than conventional GIC at baseline and 6 months follow up.
References
- Ozdemir D. Dental caries: The most common disease worldwide and preventive strategies. Int J Biol. 2013; 5(4): 55.
- Agaku IT, Olutola BG, Adisa AO, Obadan EM, Vardavas CI. Association between unmet dental needs and school absenteeism because of illness or injury among US school children and adolescents aged 6-17 years, 2011-2012. Prev Med. 2015; 72: 83-88.
[Crossref] [Google Scholar] [Pubmed]
- Skeie MS, Raadal M, Strand GV, Espelid I. The relationship between caries in the primary dentition at 5 years of age and permanent dentition at 10 years of age-a longitudinal study. Int J Paediatr Dent. 2006; 16(3): 152-160.
[Crossref] [Google Scholar] [Pubmed]
- Broadbent JM, Thomson WM, Williams SM. Does caries in primary teeth predict enamel defects in permanent teeth? A longitudinal study. J Dent Res. 2005; 84(3): 260-264.
[Crossref] [Google Scholar] [Pubmed]
- Walsh T, Worthington HV, Glenny AM, Appelbe P, Marinho VC, Shi X. Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2010; (1): CD007868.
[Crossref] [Google Scholar] [Pubmed]
- American Academy on Pediatric Dentistry (AAPD) Dental Care Programs Committee, American Academy on Pediatric Dentistry Council on Clinical Affairs. Policy on oral health care programs for infants, children, and adolescents. Pediatr Dent. 2008; 30(7): 21.
[Google Scholar] [Pubmed]
- Beltrán-Aguilar ED, Barker LK, Canto MT, Dye BA, Gooch BF, Griffin SO, et al. Surveillance for dental caries, dental sealants, tooth retention, edentulism, and enamel fluorosis-United States, 1988-1994 and 1999-2002. MMWR Surveill Summ. 2015; 54: 1-43.
[Google Scholar] [Pubmed]
- Murdoch-Kinch CA, McLean ME. Minimally invasive dentistry. J Am Dent Assoc. 2003; 134(1): 87-95.
[Crossref] [Google Scholar] [Pubmed]
- Frencken JE, Leal SC, Navarro MF. Twenty-five-year Atraumatic Restorative Treatment (ART) approach: A comprehensive overview. Clin Oral Investig. 2012; 16(5): 1337-1346.
[Crossref] [Google Scholar] [Pubmed]
- Ensaff H, O'Doherty DM, Jacobsen PH. Polymerization shrinkage of dental composite resins. Proc Inst Mech Eng H. 2001; 215(4): 367-375.
[Crossref] [Google Scholar] [Pubmed]
- Donly K. Pediatric Restorative Dentistry Consensus Conference. Pediatric Dent. 2002; 424: 24.
[Google Scholar] [Pubmed]
- Palin WM, Fleming GJ. Low-shrink monomers for dental restorations. Dent Update. 2003; 30(3): 118-122.
[Crossref] [Google Scholar] [Pubmed]
- Yap AU, Pek YS, Cheang P. Physico‐mechanical properties of a fast‐set highly viscous GIC restorative. J Oral Rehabil. 2003; 30(1): 1-8.
[Crossref] [Google Scholar] [Pubmed]
- Cehreli SB, Ebru TR, Yalcinkaya Z, Cehreli ZC. Microleakage of newly developed glass carbomer cement in primary teeth. Eur J Dent. 2013; 7(01): 15-21.
[Crossref] [Google Scholar] [Pubmed]
- Gorseta K, Glavina D, Borzabadi-Farahani A, van Duinen RN, Skrinjaric I, Hill RG, et al. One-year clinical evaluation of a glass carbomer fissure sealant, a preliminary study. Eur J Prosthodont Restor Dent. 2014; 22(2): 67-71.
[Google Scholar] [Pubmed]
- van Duinen RN, Davidson CL, de Gee AJ, Feilzer AJ. In situ transformation of glass-ionomer into an enamel-like material. Am J Dent. 2004; 17(4): 223-227.
[Google Scholar] [Pubmed]
- Hassan A, el Tekeya M, Hanafy SA, Talaat DA. Microleakage evaluation of glass carbomer cement with and without surface coat in primary molars (In vitro study). Egypt Dent J. 2016; 62(1): 515-524.
- Nassar AM, Abdalla AI, Shalaby ME. One year clinical follow up of nano filled glass ionomer and composite resin restorations. Tanta Dent J. 2014; 11(1): 21-35.
- Viera AJ, Bangdiwala SI. Eliminating bias in randomized controlled trials: Importance of allocation concealment and masking. Fam Med. 2007; 39(2): 132.
[Google Scholar] [Pubmed]
- Gorseta K, Glavina D, Skrinjaric T, Czarnecka B, Nicholson JW. The effect of petroleum jelly, light-cured varnish and different storage media on the flexural strength of glass ionomer dental cements. Acta Biomater Odontol Scand. 2016; 2(1): 55-59.
[Crossref] [Google Scholar] [Pubmed]
- HHU. G*Power: Statistical power analyses for mac and windows. Heinrich-Heine-Universität Düsseldorf (HHU). 2019.
- Gunda S, Varma N. Minimal intervention in pediatric dentistry. J Orofacial Res. 2019; 3: 28-33.
- de França CM, Schubert EW, Martins AS, Loguercio AD, Reis A, Chibinski AC, et al. Randomized clinical trial of ART Class II restorations using two glass ionomer cements: One-year follow-up. Pediatr Dent. 2018; 40(2): 98-104.
[Google Scholar] [Pubmed]
- Ekstrand KR, Martignon S, Ricketts DJ, Qvist V. Detection and activity assessment of primary coronal caries lesions: A methodologic study. Oper Dent. 2007; 32(3): 225-235.
[Crossref] [Google Scholar] [Pubmed]
- Hickel R, Roulet JF, Bayne S, Heintze SD, Mjör IA, Peters M, et al. Recommendations for conducting controlled clinical studies of dental restorative materials. Clin Oral Investig. 2007; 11(1): 5-33.
[Crossref] [Google Scholar] [Pubmed]
- Moszner N, Klapdohr S. Nanotechnology for dental composites. Int J Nanotechnol. 2004; 1(1-2): 130-156.
- Croll TP, Nicholson JW. Glass ionomer cements in pediatric dentistry: Review of the literature. Pediatr Dent. 2002; 24(5): 423-429.
[Google Scholar] [Pubmed]
- Cehreli ZC, Gungor HC. Quantitative microleakage evaluation of fissure sealants applied with or without a bonding agent: Results after four-year water storage in vitro. J Adhes Dent. 2008; 10(5): 379-384.
[Crossref] [Google Scholar] [Pubmed]
- Derkson GD, Richardson AS, Waldman R. Clinical evaluation of composite resin and amalgam posterior restorations: Two year results. J Can Dent Assoc. 1983; 49(4): 277-279.
[Google Scholar] [Pubmed]
- Feilzer AJ, de Gee AJ, Davidson CL. Setting stresses in composites for two different curing modes. Dent Mater. 1993; 9(1): 2-5.
[Crossref] [Google Scholar] [Pubmed]
- Aboush YE, Jenkins CB. The effect of poly (acrylic acid) cleanser on the adhesion of a glass polyalkenoate cement to enamel and dentine. J Dent. 1987; 15(4): 147-152.
[Crossref] [Google Scholar] [Pubmed]
- Wilson AD. A survey of inorganic and polyelectrolyte cements. Br Dent J. 1984; 157: 449-454.
[Crossref] [Google Scholar] [Pubmed]
- Mount GJ. Glass-ion omer restorative cements: Clinical-implications of the setting reaction. Oper Dent. 1982; 7: 134-141.
[Google Scholar] [Pubmed]
- Asmussen E. Opacity of glass-ionomer cements. Acta Odontol Scand. 1983; 41(3): 155-157.
[Crossref] [Google Scholar] [Pubmed]
- Earl MS, Hume WR, Mount GJ. Effect of varnishes and other surface treatments on water movement across the glass‐ionomer cement surface. Aust Dent J. 1985; 30(4): 298-301.
[Crossref] [Google Scholar] [Pubmed]
- Rodrigues RCG, de Goes MF, del Cury AA. Influence of protecting agents on the solubility of glass ionomers. Am J Dent. 1995; 8(6): 294-296.
[Google Scholar] [Pubmed]
- Moshaverinia A, Roohpour N, Chee WW, Schricker SR. A review of powder modifications in conventional glass-ionomer dental cements. J Mater Chem. 2011; 21(5): 1319-1328.
- Watson T, Banerjee A. Effectiveness of glass-ionomer surface protection treatments: A scanning optical microscope study. Eur J Prosthodont Restor Dent. 1993; 2(2): 85-90. [Crossref]
[Google Scholar] [Pubmed]
Author Info
Amr H Ali1*, Ahmed A Mohamed2 and Dalia M Talaat12Department of Pediatric Dentistry and Dental Public Health, Alexandria University, Alexandria, Egypt
Citation: Ali AH: Effectiveness of Ketac Nano Restoration in Class II Cavities in Primary Molars: A Randomized Controlled Clinical Trial
Received: 02-Dec-2022 Accepted: 27-Dec-2022 Published: 03-Jan-2023, DOI: 10.31858/0975-8453.14.1.11-18
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3