Research Article - (2024) Volume 15, Issue 4
Emergence of Syphilis Infection beyond HIV Infection as More Relevant Indicator for Hepatitis C Virus Infection Susceptibility
Cynthia Turner1,2*, Tuan Phan2, OsaroMgbere1, Jennifer Perez1 and Lupita Thornton1Abstract
Objective: Observations at the Houston Health Department revealed that syphilis infection has potentially emerged beyond Human Immunodeficiency Virus (HIV) infection as a highly relevant indicator of susceptibility to sexually transmitted Hepatitis C Virus (HCV) infection. Identification of syphilis as a relevant predictive indicator of HCV infection susceptibility may facilitate optimization of diagnostic algorithms for HCV detection among targeted populations.
Methods: A multifaceted proof of concept study compared the prevalence of syphilis co-infection to HIV co-infection among individuals with Hepatitis C Virus antibody (HCVab). Remnant serum samples previously tested for HIV and syphilis were analyzed for HCVab presence using an Enzyme-Linked Immunosorbent Assay (ELISA). Conversely, remnant HCVab positive samples were analyzed for syphilis and HIV infection using conventional diagnostic assays. The independent associations between data sources of positive cases and demographic characteristics (gender, age category and race/ethnicity) were determined using the Chi-square (χ2) test or Fisher test where cases were <5. Prevalence of HCV, HIV and syphilis infections and its associated co-infections by demographic characteristics were assessed using the Chi-square test. Predictive screening and ranking of independent factors and the associated relative risks of HCV, HIV and syphilis infection diagnosis and co-infections with HCV were also determined. All statistical tests performed were 2-tailed with a p-value, 0.05 as statistical significance. Data management and statistical analysis was conducted using JMP (statistical software) version 14.3 (SAS Institute, Cary, North Carolina, USA).
Results: Assessment of the association of mono- and co-infection with HIV, syphilis and HCV among the study individuals was statistically relevant (p<0.0001). Overall, 8.22% of the study samples were HCV/syphilis co-infected compared to 1.37% HCV/HIV co-infected.
Conclusion: The prevalence of HCV/syphilis co-infection far exceeded prevalence of HCV/HIV co-infection in this study. This may be attributed, in part, to advances in HIV treatment which lead to undetectable levels of HIV. Identification of syphilis infection, confirmed by T. pallidum seropositivity, may serve as a highly relevant predictor of HCV infection susceptibility in the absence of identifiable HIV infection, thereby proving to be an efficacious diagnostic tool in the early detection, intervention and treatment of HCV infection.
Keywords
Hepatitis C virus, Co-infection, HIV, Syphilis, Sexually Transmitted Infection (STI)
Introduction
Significant attention has been given to the concept that infection with Human Immunodeficiency Virus (HIV) is a relevant indicator when predicting susceptibility to Hepatitis C Virus (HCV) infection (World Health Organization, 2017; Platt L, et al., 2016; Sulkowski MS, 2012). Some studies have reported that people living with HIV can be anywhere from twice as likely to six times more likely to be co-infected and/or re-infected with HCV (Platt L, et al., 2016; Hagan H, et al., 2015; Schroeder SE, et al., 2019). The increased susceptibility to HCV co-infection in people living with HIV is noted as especially significant among Men who have Sex with Men (MSM), as well as gay and bisexual men (Hagan H, et al., 2015; Schroeder SE, et al., 2019; Moorman JP, et al., 2018). The notion of increased susceptibility to HCV infection in individuals that have a positive HIV status asserts that all samples submitted for HIV antibody testing should also be tested for HCV antibody to bolster intervention, education and, prevention strategies for HCV (Martin TC, et al., 2018; Lu T, et al., 2013).
For years, HCV intervention and education strategies were directed at individuals born during the years of 1945 and 1965, the generation known as the Baby Boomers. Subsequently, the Centers for Disease Control and Prevention (CDC) and the US Preventive Services Task Force (USPSTF) have recommended that all individuals that were born between those years be tested for HCV (Geboy AG, et al., 2016; Centers for Medicare and Medicaid Services, 2014; Moyer VA, 2013). In terms of public health jargon, the Baby Boomer generation is categorically defined as the HCV birth cohort (Smith BD, et al., 2012). Up to now, this cohort has served as the gold standard of measurement for HCV infection within a population. Increased testing and reporting of HCV results have shown that more and more individuals that fall below the age range of the HCV birth cohort are infected with HCV, thereby invalidating the birth cohort as the standard for measuring population prevalence of HCV infection.
It has been well established that social behavior plays a significant role in the infection and transmission of Sexually Transmitted Infections (STIs). Numerous research articles have pointed to the relationship between high-risk behaviors, such as multiple sex partners and intravenous drug use, as factors that play significant roles in contracting and transmitting HIV and syphilis (Terrault NA, et al., 2002; Feldman JG, et al., 2000; Nurutdinova D, et al., 2011; Su S, et al., 2018; Ng’wamkai G, et al., 2019; Shimelis T, et al., 2017). It has also been shown that infection with HIV is a highly relevant indicator that one would also become co-infected with HCV (Soriano V, et al., 2006; Ayele W, et al., 2002). A concept that warrants consideration is the co-infection relationship between syphilis and sexually transmitted HCV, since both infections most likely result from similar social behaviors.
Findings of the current study deviates from the accepted theory that HIV infection is the most relevant indicator of susceptibility for co-infection with HCV. Unlike many earlier studies that assert that HIV co-infection is the premier indicator for susceptibility to HCV infection, the current proof of concept study reveals that in the assessed geographic region, syphilis infection, confirmed by a positive Treponema pallidum serostatus has emerged as a more relevant marker for prediction of susceptibility to HCV infection rather than the presence of HIV infection.
Thus, the objective of this study is to assess the co-infection correlation between syphilis and HCV in the Houston and greater Houston areas.
Materials and Methods
Detection of hepatitis C virus antibody
Remnant serum samples that had been stored frozen at -80°C in capped 12 × 75 mm polypropylene test tubes were thawed and allowed to come to ambient temperature. Samples were screened (analyzed) for the presence of antibodies to HCV using the ORTHO® HCV version 3.0 ELISA test system assay. The assay is a qualitative, enzyme-linked immunosorbent assay, in which a 5% (1/20) dilution of the sample is analyzed to detect the presence of HCV antibody. The serum sample was diluted using the test kit diluent. The assay was carried out on a 96-well microplate that was pre-coated with three yeast-derived recombinant HCV antigens. The assay was performed according to the manufacturer’s package insert on the BioRad EVOLIS™ system, a 96-well microplate automated analyzer (Ortho clinical diagnostics, 2009).
Data abstraction from historical records
A query was performed in the Houston Health Department (HHD) Laboratory Information System (LIS) database to search for previously tested samples that were reported with a positive result for the HCV antibody during the years of 2017 to 2019. An ad hoc report with defined demographic parameters was generated within the search and was printed for review and analysis. All relevant data from the ad hoc report, including age, gender, race/ethnicity, and diagnostic test results (HCV antibody, HIV, and syphilis assay), were transferred to an Excel spreadsheet for analysis.
Supplemental testing for determining the prevalence of HIV and syphilis coinfection
HIV testing: Study samples that were positive for the presence of HCV antibodies were assessed for co-infection with HIV. Testing for HIV status was carried out using the BioPlex®2200 system HIV Ag-Ab (test kit and analyzer). The assay is a multiplex flow immunoassay. The technology involves combining an aliquot of the sample with four populations of monoclonal antibody-coated dyed beads. The final analysis is accomplished using fluorescence technology. The assay is qualitative, and it simultaneously detects the presence of HIV-1 p24 antigen, antibodies to HIV-1 (groups M and O), and HIV-2 antibodies in a single sample. The assay was performed on the BioPlex® 2200 system analyzer, and according to the manufacturer’s package insert (BioRad, 2015).
Samples that yielded a positive result for any of the HIV analytes detected by the BioPlex® 2200 System HIV Ag-Ab assay were then analyzed using the GEENIUS™ HIV1/2 supplemental assay, manufactured by BioRad, to determine the final HIV infection status (HIV positive or HIV negative). The assay serves to differentiate HIV analytes (antibody to HIV-1 or HIV- 2, HIV-1 antigen). It employs immunochromatographic technology, and it was performed according to the manufacture’s package insert (BioRad, 2015).
Syphilis testing: Samples that were identified as positive for HCV antibodies (via screening and data abstraction) that did not have a historical record of syphilis testing in the LIS were assessed for syphilis infection using the ASI™ RPR card test for syphilis (manufactured by Arlington Scientific, Inc.). The assay is a qualitative and semi-quantitative nontreponemal flocculation assay. It was performed according to the manufacturer’s package insert (Arlington Scientific, 2014). Samples that were reactive by the RPR test were confirmed for syphilis infection viaqualitative assessment using the Fujirebio Serodia TP-PA® treponemal assay to confirm a positive Treponema pallidum serostatus. The assay is a qualitative gelatin particle agglutination assay that can detect antibodies to T. pallidum. It was performed according to the manufacturer’s package insert. A reactive RPR result, along with a positive TP-PA assay result, is indicative of syphilis infection (NHANES, 2001).
Statistical analysis
All the diagnostic testing and record abstraction data were entered into Excel spreadsheets that were labeled by the focus of the content. A separate spreadsheet was utilized for each diagnostic test experiment set. The data from the individual experiment sets were then combined into a single table for comparison. Likewise, a separate spreadsheet was constructed for each year of historical record search data abstraction. The data from the separate years were then combined into a single table for comparison. Bi- variate analyses using the Chi-square test was conducted to determine the independent associations among the infections (HCV, HIV and syphilis), co-infections (HCV/HIV and HCV/syphilis), and demographic characteristics (gender, age category, and race/ethnicity). All statistical tests performed were 2-tailed, with a probability value of 0.05 used as the threshold for declaring statistical significance. Data management and statistical analyses were conducted using SAS JMP Statistical DiscoveryTM software version 14.3 (SAS Institute, Cary, North Carolina, USA).
Results
Co-existence of positive T. pallidum serostatus vs. positive HIV status among HCV antibody positive cross-sectional test samples
A total of 811 viable results were obtained from four cross-sectional experiment sets that were tested for the presence of HCV antibody. The sets were labeled as routine syphilis set, RPR reactive set, TP-PA set 1 and TP-PA set 2. HCV antibody was detected in 2.6% (21/811) of the samples. The aggregate of the gender composition of the combined cross-sectional experiment sets was 63.3% (513/811) male and 36.7% (298/811) female. Black males accounted for 38.1% (8/21) of all HCV antibody (HCVab) positive samples, followed by black females at 23.8% (5/21). The distribution of males by race/ethnicity was found to be 45.2% (232/513) black, 46.8% (240/513) Hispanic, 5.5% (28/513) white and 2.5% (13/513) other or unknown race/ethnicity. The distribution of female samples that were: 50.7% (151/298) black, 46.6% (139/298) Hispanic, 1.3% (4/298) white and 1.3% (4/298) of other or unknown race/ethnicity. When comparing positive HCV antibody results of males and females was 2.9% (15/513) of males were positive for HCV antibody presence compared to 2.0% (6/298) of females. African American males and females showed similar rates of HCV antibody presence at 3.4% and 3.3%, respectively. Likewise, Hispanic males and females had comparable rates of HCV antibody presence at 0.8% and 0.7%, respectively. The sample volume of white males and females was low; however, white males had a significantly higher rate of HCV antibody presence (14.3%) than white females (0%). Males and females of other or unknown race/ethnicity showed HCV antibody presence at 7.7% and 0% respectively. Results for other/unknown race/ethnicity were treated discriminately with the exception of when assessing aggregated results that excluded race/ethnicity to prevent skewing of results since they are most likely a member of one of the other race/ethnicity groups but were not identified during the sample submission or accessioning process. Table 1, summarizes the results of the cross-sectional testing experiment sets by the demographics of gender and race/ethnicity. A total of 66.7% (14/21) of the HCV antibody-positive samples had co-existence of a positive T. pallidum serostatus. The co-existence of a positive HIV status was present in 9.5% (2/21) of the HCV antibody-positive samples. The rate of positive HCV- ab/positive T. pallidum serostatus co-existence was 100% (5/5) among the African American females tested in this experiment set vs. zero percent positive HCVab/positive HIV status co-existence among black females and females of Hispanic and white race/ethnicity. Positive HCVab/positive T. pallidum serostatus co-existence was 75% (6/8) among the black males tested in this experiment set, vs. 12.5% (1/8) positive HCVab/positive HIV status co-existence among black males. Hispanic males all had the co-existence of a positive T. pallidumserostatus. Hispanic males did not have a positive HIV status. White males in this experiment set did not have positive serostatus for T. pallidumor HIV (Table 2). In general, males accounted for 71.4% (15/21) of the HCV antibody-positive samples, and females accounted for 28.6% (6/21). Black males accounted for 53.3% (8/15) of the HCV antibody-positive males, of which 75% (6/8) of the black males had co-existence of a positive T. pallidum serostatus and 12.5% (1/8) were co-infected with HIV. Hispanic males accounted for 13.3% (2/15) of the HCV antibody-positive males. Both Hispanic males were seropositive for T. pallidum, but neither was infected with HIV. White males accounted for 26.7% (4/15) of the HCV antibody-positive males. Neither was seropositive for T. pallidumor HIV. There was one male of other or unknown race/ ethnicity that tested positive for the presence of HCV antibodies. The sample was also T. pallidumseropositive and positive for HIV infection. Black females comprised 83.3% (5/6) of HCV antibody-positive females, and 100% (5/5) of the black females were T. pallidum seropositive. Neither of the black females was co-infected with HIV. Hispanic females comprised 16.7% (1/6) of the female HCV antibody-positive samples. The Hispanic female was not positive for T. pallidumor HIV. No white females in this component of the study exhibited the presence of HCV antibodies.
| HCV antibody screening | % HCV antibody positive | |
|---|---|---|
| No. of samples | ||
| Total samples | 811 | 2.6 (21/811) |
| Males | 513 | 2.9 (15/513) |
| Females | 298 | 2.0 (6/298) |
| Black males | 232 | 3.4 (8/232) |
| Hispanic males | 240 | 0.8 (2/240) |
| White males | 28 | 14.3 (4/28) |
| Other/unknown males | 13 | 7.7 (1/13) |
| Black females | 151 | 3.3 (5/151) |
| Hispanic females | 139 | 0.7 (1/139) |
| White females | 4 | 0 |
| Other/unknown females | 4 | 0 |
Table 1: HCV antibody screening results for samples that were previously submitted for syphilis testing
| Assessment based on ethnicity | HCV antibody positive | % syphilis co-infected | |
|---|---|---|---|
| No. of samples | % HIV co-infected | ||
| Total samples | 21 | 9.5 (2/21) | 66.7 (14/21) |
| Male | 15 | 13.3 (2/15) | 60 (9/15) |
| Female | 6 | 0 | 83.3 (5/6) |
| Black males | 8 | 12.5 (1/8) | 75 (6/8) |
| Hispanic males | 2 | 0 | 100 (2/2) |
| White males | 4 | 0 | 0 |
| Other/unknown males | 1 | 100 (1/1)* | 100 (1/1)* |
| Black females | 5 | 0 | 100 (5/5) |
| Hispanic females | 1 | 0 | 0 |
| White females | 0 | 0 | 0 |
| Other/unknown females | 0 | 0* | 0* |
Note: *Results of other/unknown race/ethnicity group will not be considered independently in the overall analysis of the study, but only as part of the aggregate number of HCV antibody positive samples
Table 2: Assessment of positive T. pallidum serostatus co-existence vs. positive HIV status co-existence by gender and race/ethnicity among samples that were HCV antibody positive
Of all the HCV antibody-positive males that fell below the birth cohort, 50% (5/10) of the samples were black males, of which 40% (2/5) had co-existence of a positive T. pallidumserostatus, and 20% (1/5) had dual co-existence of positive T. pallidumand HIV serostatus. 50% (1/2) of HCV antibody Hispanic males fell below the birth cohort. The Hispanic male was T. pallidumseropositive but negative for HIV infection. In terms of females that fell below the birth cohort that had HCV antibodies present, two were blacks, and both, 100% (2/2), were T. pallidumseropositive. Neither of the two black females that fell below the cohort was positive for HIV infection. There were no white females below the birth cohort that exhibited the presence of HCV antibodies.
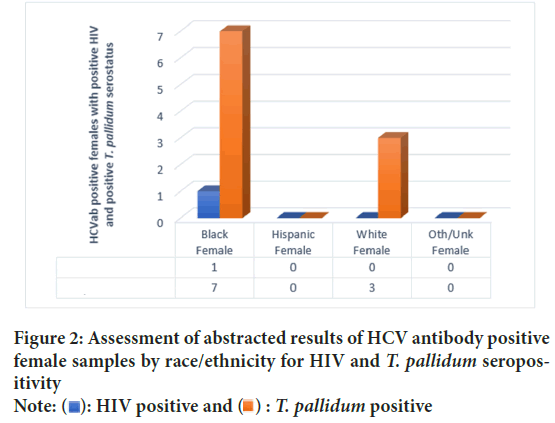
Data abstraction and supplemental testing of remnant samples to examine prevalence of HIV and T. pallidum seropositivity among HCV antibody samples
A historical record search of the HHD laboratory information system for results of HCV antibody-positive samples detected from 2017 through 2019 was performed, and 417 HCV antibody-positive samples were identified. Many of the identified HCVab positive samples from this search were associated with a prior study that targeted specific confounding factors for HCV infection, and no HIV or syphilis testing was performed on them. HCVab results from samples associated with that study were excluded from the analysis of the results of the current study; thereby, resulting in 284 viable results from the record abstraction. The samples were examined to assess the prevalence of co-existence of a positive HIV status and positive T. pallidum serostatus among the HCVab positive samples. Supplemental testing to determine T. pallidum and HIV serostatus among HCVab positive samples that had not been previously tested for those analytes was conducted on remnant samples. Data abstraction and supplemental testing revealed that 30% (84/284; 74 males, 10 females) of the samples had co-existence of a positive T. pallidumserostatus, and 5% (14/284; 10 males, 4 females) had co-existence of a positive HIV status. The positive HIV and T. pallidumco-existence prevalence among those samples is depicted in (Figure 1 and Figure 2) for males and females, respectively.
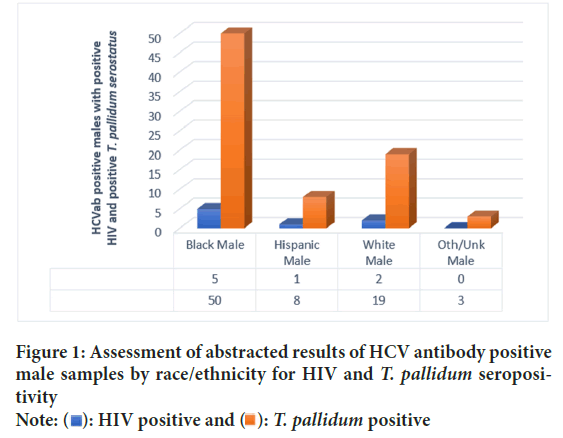
Figure 1: Assessment of abstracted results of HCV antibody positive male samples by race/ethnicity for HIV and T. pallidum seropositivity
Note:  : HIV positive and
: HIV positive and  : T. pallidum positive
: T. pallidum positive
Figure 2: Assessment of abstracted results of HCV antibody positive female samples by race/ethnicity for HIV and T. pallidum seropositivity
Note:  : HIV positive and
: HIV positive and  : T. pallidum positive
: T. pallidum positive
When comparing the prevalence of T. pallidum and HIV co-existence among males and females within the same race/ethnicity from the abstracted results data and supplemental testing: 37% (48/130) of HCV antibody-positive black males were T. pallidum seropositive, compared to 13.5% (7/52) black females. For HIV co-infection, 4.6% (6/130) of African American men tested were co-infected with HIV compared to 5.8% (3/52) of African American females. In comparing results from Hispanic individuals: 46.7% (7/15) of Hispanic males were T. pallidumseropositive vs. 0% (0/1) Hispanic females. HIV-positive Hispanic males and females existed at 6.7% (1/15) and 0%, respectively. Among white males, 30.6% (15/49) were seropositive for T. pallidumcompared to 16.7% (3/18) of white females. In terms of HIV co-infection, 4.1% (2/49) of white men were co-infected, and 5.6% (1/18) of white females (Figure 3).
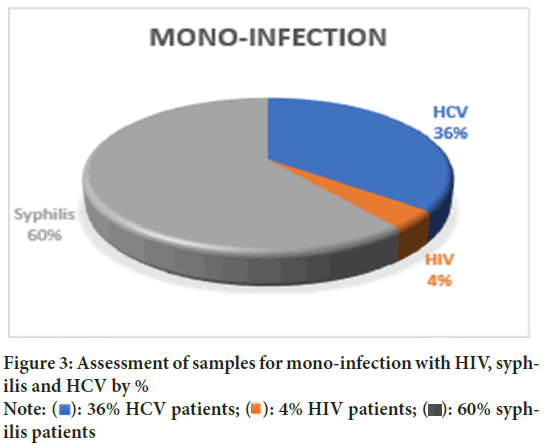
Figure 3: Assessment of samples for mono-infection with HIV, syphilis and HCV by %
Note:  : 36% HCV patients;
: 36% HCV patients;  : 4% HIV patients;
: 4% HIV patients;  :60% syphilis patients
:60% syphilis patients
Aggregate analysis of combined study components: Bivariate analysis using the Chi-squared test was performed to assess the overall results of the combined components of the study.
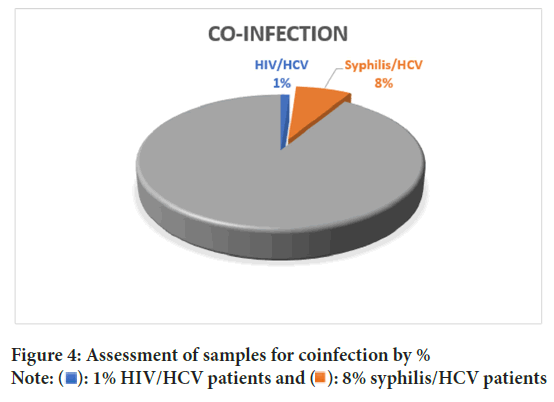
Samples that did not possess results for all three analytes of interest (HCV, HIV, and T. pallidum) were eliminated from the analysis. Independent association and co-infection, among the analytes, were statistically relevant (p<0.0001) and is shown in (Table 3). Syphilis infection among the analyzed samples was 94.16% (p<0.0001), and HCV and HIV rates of infection were 26.78% and 3.14%, respectively. Co-infection rates of the combined cross-sectional experiment sets, and historical record data abstraction, revealed that overall, 8.22% of the samples were HCV/syphilis co-infected compared to 1.37% HCV/HIV co-infected as shown in (Figure 4). Less than 1% of the HCVab positive samples were dually co-infected with HIV and syphilis.
| Study components | Sample | Positive | Negative | Test statistics | |
|---|---|---|---|---|---|
| Infection | n | n (%) | n (%) | χ2 | p-value |
| HCV | 1079 | 289 (26.78) | 790 (73.22) | 232.62 | <0.0001**** |
| HIV | 1020 | 32 (3.14) | 988 (96.86) | 896.02 | <0.0001**** |
| Syphilis | 514 | 484 (94.16) | 30 (5.84) | 401 | <0.0001**** |
| Co-infection | Yes | No | χ2 | p-value | |
| HCV+HIV | 1095 | 15 (1.37) | 1080 (98.63) | 1035.82 | <0.0001**** |
| HCV+syphilis | 1095 | 90 (8.22) | 1005 (91.78) | 764.59 | <0.0001**** |
| HCV+HIV+syphilis | 1095 | 8 (0.73) | 1087 (99.27) | 1063.23 | <0.0001**** |
Table 3: Bivariate analysis of the combined study components comparing independent association and co-infection rates among HCV, HIV and syphilis
Figure 4: Assessment of samples for coinfection by %
Note:  : 1% HIV/HCV patients and
: 1% HIV/HCV patients and  : 8% syphilis/HCV patients
: 8% syphilis/HCV patients
Discussion
Infection with Hepatitis C virus has far-reaching relevance in public health, with reported global infection rates of more than 150 million people. Of great concern is that many cases go undetected because only about 25% of infected individuals are symptomatic (Bukh J, 2016). Further compounding the issue of asymptomatic infection is the failure of treatment in 2.5%- 5% of individuals, due largely to random point mutations in the genome that can confer drug resistance (Esposito I, et al., 2018). This multifaceted proof of concept study aimed to bring attention to the relevance of syphilis infection as a predictive factor for HCV infection susceptibility compared to the relevance of HIV infection. Samples in the cross-sectional component of the study had been previously submitted for routine syphilis testing, but they had not been previously analyzed for the presence of HCV antibodies. In the first cross-sectional experiment set, randomly selected samples that had been previously submitted for routine syphilis testing were analyzed for the presence of HCV antibody using an ELISA based assay. Initially, 491 samples were randomly selected for this experiment set; however, 26 samples were eliminated due either to insufficient demographic information or insufficient volume; thereby, yielding 465 viable results. The presence of HCV antibody was detected in 2.2% (10/465) of the sample sets, and 30% (3/10) of the HCV antibody-positive samples of this set were T. pallidumseropositive, whereas 0% of the samples were co-infected with HIV. The second experiment set in the cross-sectional component consisted of specimens that had been submitted for routine syphilis testing and were reactive by the nontreponemal, Rapid Plasma Reagin (RPR) syphilis screening assay but may not have yet been confirmed for syphilis infection by a treponemal assay. There were 160 samples in this set, and 3.1% were positive for HCV antibody presence. Of those samples that had HCV antibody present, 100% (5/5) had a positive T. pallidumserostatus, and 0% were positive for co-infection with HIV. Four of the five HCV antibody-positive samples were African American females, and 100% (4/4) of the African American females were Treponema pallidum seropositive. The fifth HCV antibody-positive sample was a Hispanic male. The experiment set labeled TP-PA set 1 consisted of 97 samples, of which 5.2% (5/97) had HCV antibodies present. All five HCV positive samples were male (3 African American, 1 Hispanic, 1 unknown race/ethnicity); 100% (5/5) were TP-PA positive, and 40% (2/5) were co-infected with HIV. The HIV positive samples were dually co-infected with HIV and syphilis, and they fell below the HCV birth cohort. Active syphilis infection in these samples was determined by a reactive nontreponemal assay (RPR) that was confirmed by a treponemal assay, TP-PA. The TP-PA Set 2 experiment set consisted of 89 samples, of which 1.1% (1/89) was positive for HCV antibodies. The HCV positive sample was an African American female who was also T. pallidum seropositive and not co-infected with HIV. Overall, 66.7% of HCV antibody-positive samples that were detected among the 811 remnant syphilis submission samples had a positive Treponema pallidum serostatus; however, only 9.5% of those HCV antibody-positive samples showed co-infection with HIV. Additionally, 100% of the African American women that were HCV antibody positive also had a positive Trepon- ema pallidumserostatus, but none of the African American women were co-infected with HIV. This was the case in all African American women, including those that fell below the birth cohort. Although black males and females had a similar incidence of HCV positivity, black females had a higher incidence (100%) of the co-existence of HCV antibody/T. pallidum seropositivity, than HCVab positive black males, of which exhibited T. pal- lidumco-existence at 75% (Ufearo H, et al., 2010; Jewett A, et al., 2013).
A record search of the HHD laboratory information system database was performed to identify and abstract results for samples that had been specifically submitted for HCV testing during the years of 2017 through 2019 and that had HCV antibody-positive results. There were 417 samples identified as positive for HCV antibodies. Many of the identified HCVab positive samples from this search were associated with a prior study that targeted specific confounding factors for HCV infection, and no HIV or syphilis testing was performed on them. Remnants for many of the samples could not be located for supplemental testing to determine HIV and T. pallidumserostatus; therefore, samples for which no remnants were located were excluded from the final analysis of the current study; thereby, resulting in 284 viable results from the record abstraction. Additionally, HCV chronically infected samples were identified viarecord abstraction. Chronic infection was determined by the existence of positive results for the HCV Nucleic Acid Amplification Test (HCV NAAT) for the sample.
Abstracted results were examined to identify samples that were co-infected with syphilis and HIV. Overall, 35.7% (74/207) of HCV positive males were co-infected with syphilis, and 4.8% (10/207) were co-infected with HIV. For females, 13.7% (10/73) were co-infected with syphilis, and less than 5.5% (4/73) were infected with HIV. When comparing the prevalence of co-infection with syphilis among all abstracted records of females that were HCV antibody positive was 13.5% (7/52) of African American women had a positive Treponema pallidumserostatus compared to 0% of Hispanic women and 16.7% (3/18) of Caucasian females.
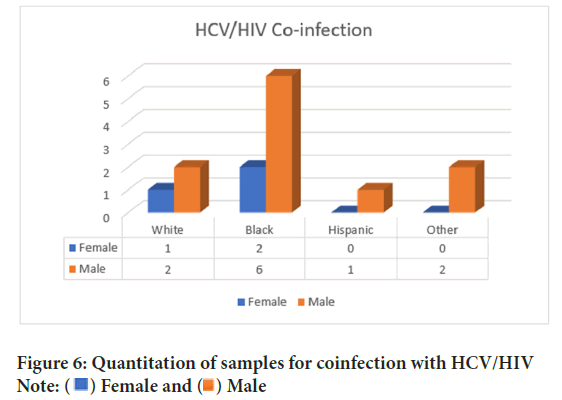
Analysis of the aggregated results of the study demonstrates that African American (Black) men have a high incidence of syphilis co-infection in the presence of other STIs. It is noteworthy to point out that in this study, we also observed marked syphilis infection among Hispanic men. When examining HCV/syphilis co-infection among women, African American females had a significantly higher incidence (21.1%) than Hispanic and white women (0% and 16.7%, respectively). It should also be noted that whereas African American and Caucasian (White) females exhibit similar incidence of HCV/HIV co-infection in this study, HCV antibody-positive Black women that were HIV positive were always dually co-infected with syphilis; whereas white women were either mono-infected with HCV, or when co-infected with syphilis, they were not co-infected with HIV as well (Figure 5 and Figure 6). Even in the presence of HIV-co-infection, African American women in this study also had a positive Treponema pallidum serostatus indicating HCV/HIV/syphilis multi-infection.
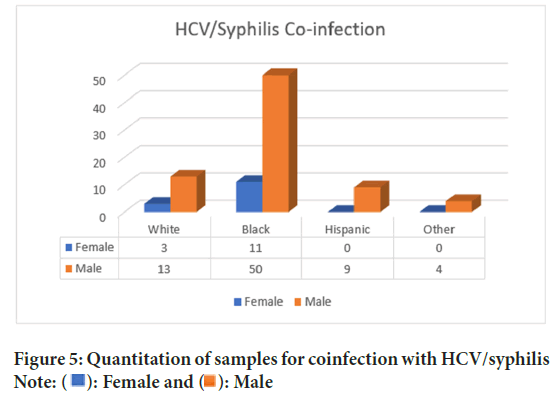
Figure 5: Quantitation of samples for coinfection with HCV/syphilis
Note:  : Female and
: Female and  : Male
: Male
Figure 6: Quantitation of samples for coinfection with HCV/HIV
Note:  Female and
Female and  Male
Male
One published study that was reviewed related to the spontaneous clearance of HCV infection in the presence of HIV co-infection may shed some light on this multi-infection phenomenon among African American women as the study proposes that African American women are less likely than Hispanic and Caucasian women to spontaneously resolve HCV infection and are thus more prone to developing chronic HCV infections than Hispanic and white women (Randall G, et al., 2003; Sarkar M, et al., 2013).
Conclusion
In the grand scheme of relevant public health information, there is no question that HIV and syphilis play complementary roles as predictive markers of co-infection for various sexually transmitted infections; however, increased attention should be directed toward the role, and significance, of syphilis infection as a predictive indicator of susceptibility to HCV infection. The prevalence of HCV/syphilis co-infection far exceeded prevalence of HCV/HIV co-infection in this study. This may be attributed, in part, to advances in HIV treatment which lead to undetectable levels of HIV antibody. Identification of syphilis infection, confirmed by T. pal- lidumseropositivity, may serve as a highly relevant predictor of HCV infection susceptibility in the absence of identifiable HIV infection; thereby, proving to be an efficacious diagnostic tool in the early detection, intervention, and treatment of HCV infection. This study clearly supports the theory that syphilis has indeed emerged as the more relevant predictive marker for co-infection with HCV across all demographics as compared to HIV infection. This is especially relevant among African American women because this group exhibits syphilis co-infection with and without HIV co-infection. The outcomes revealed in this study should be further investigated and strongly considered when devising intervention, education, and prevention strategies for HCV infection.
Limitations of Study
Sample selection was limited to individuals that utilize the HHD public health system for routine STI diagnosis. Location of remnant samples for supplemental testing also posed some limitations.
References
- Global hepatitis report 2017. World Health Organization (WHO). 2017.
- Platt L, Easterbrook P, Gower E, McDonald B, Sabin K, McGowan C, et al. Prevalence and burden of HCV co-infection in people living with HIV: A global systematic review and meta-analysis. Lancet Infect Dis. 2016; 16(7): 797-808.
[Crossref] [Google scholar] [Pubmed]
- Sulkowski MS. Hepatitis C virus‐human immunodeficiency virus coinfection. Liver Int. 2012;32: 129-134.
[Crossref] [Google scholar] [Pubmed]
- Hagan H, Jordan AE, Neurer J, Cleland CM. Incidence of sexually transmitted hepatitis C virus infection in HIV-positive men who have sex with men. AIDS. 2015; 29(17): 2335-2345.
[Crossref] [Google scholar] [pubmed]
- Schroeder SE, Higgs P, Winter R, Brown G, Pedrana A, Hellard M, et al. Hepatitis C risk perceptions and attitudes towards reinfection among HIV‐diagnosed gay and bisexual men in Melbourne, Australia. J Int AIDS. 2019; 22(5).
[Crossref] [Google scholar] [Pubmed]
- Moorman JP, Krolikowski MR, Mathis SM, Pack RP. HIV/HCV co-infection: Burden of disease and care strategies in Appalachia. Curr HIV/AIDS Rep. 2018; 15: 308-314.
[Crossref] [Google scholar] [Pubmed]
- Martin TC, Rauch A, Salazar-Vizcaya L, Martin NK. Understanding and addressing hepatitis C virus reinfection among men who have sex with men. Infect Dis Clin North Am. 2018; 32(2): 395-405.
[Crossref] [Google scholar] [Pubmed]
- Lu T, Seto WK, Zhu RX, Lai CL, Yuen MF. Prevention of hepatocellular carcinoma in chronic viral hepatitis B and C infection. World J Gastroenterol. 2013; 19(47): 8887.
[Crossref] [Google scholar] [Pubmed]
- Geboy AG, Mahajan S, Daly AP, Sewell CF, Fleming IC, Cha HA, et al. High hepatitis C infection rate among baby boomers in an urban primary care clinic: Results from the HepTLC initiative. Public Health Rep. 2016; 131(2_suppl):49-56.
[Crossref] [Google scholar] [Pubmed]
- Decision memo for screening for Hepatitis C Virus (HCV) in adults (CAG-00436N). Centers for medicare and medicaid services. 2014.
- Moyer VA. Screening for hepatitis C virus infection in adults: US preventive services task force recommendation statement. Ann Intern Med. 2013; 159(5): 349-57.
[Crossref] [Google Scholar] [Pubmed]
- Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Teo CG, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Recomm Rep. 2012; 61: 1-32.
[Google scholar] [Pubmed]
- Terrault NA. Sexual activity as a risk factor for hepatitis C. Hepatology. 2002; 36: 99-105.
[Crossref] [Google scholar] [Pubmed]
- Feldman JG, Minkoff H, Landesman S, Dehovitz J. Heterosexual transmission of hepatitis C, hepatitis B, and HIV-1 in a sample of inner-city women. Sex Transm Dis. 2000; 27(6): 338-342.
[Crossref] [Google scholar] [Pubmed]
- Nurutdinova D, Abdallah AB, Bradford S, O'Leary CC, Cottler LB. Risk factors associated with hepatitis C among female substance users enrolled in community-based HIV prevention studies. BMC Res Notes. 2011; 4: 1-9.
[Crossref] [Google scholar] [Pubmed]
- Su S, Mao L, Zhao J, Chen L, Jing J, Cheng F, et al. Epidemics of HIV, HCV and syphilis infection among synthetic drugs only users, heroin-only users and poly-drug users in Southwest China. Sci Rep. 2018; 8(1): 6615.
[Crossref] [Google scholar] [Pubmed]
- Ng’wamkai G, Msigwa KV, Chengula D, Mgaya F, Chuma C, Msemwa B, et al. Treponema pallidum infection predicts sexually transmitted viral infections (hepatitis B virus, herpes simplex virus-2, and human immunodeficiency virus) among pregnant women from rural areas of Mwanza region, Tanzania. BMC Pregnancy Childbirth. 2019; 19: 1-13.
[Crossref] [Google scholar] [Pubmed]
- Shimelis T, Tassachew Y, Tadewos A, Hordofa MW, Amsalu A, Tadesse BT, et al. Coinfections with hepatitis B and C virus and syphilis among HIV-infected clients in Southern Ethiopia: A cross-sectional study. HIV AIDS. 2017; 9: 203-210.
[Crossref] [Google scholar] [Pubmed]
- Soriano V, Barreiro P, Nunez M. Management of chronic hepatitis B and C in HIV-coinfected patients. J Antimicrob Chemother. 2006; 57(5): 815-818.
[Crossref] [Google scholar] [Pubmed]
- Ayele W, Nokes DJ, Abebe A, Messele T, Dejene A, Enquselassie F, et al. Higher prevalence of anti‐HCV antibodies among HIV‐positive compared to HIV‐negative inhabitants of Addis Ababa, Ethiopia. J Med Virol. 2002; 68(1): 12-17.
[Crossref] [Google scholar] [Pubmed]
- Hepatitis C virus encoded antigen (Recombinant c22-3, c200 and NS5) ORTHO® HCV version 3.0 ELISA test system. Ortho clinical diagnostics (USA). 2009.
- BioPlex 2200 system HIV Ag-Ab instructions for use. BioRad (USA). 2015.
- GEENIUS™ HIV 1/2 confirmatory assay. BioRad (USA). 2015.
- ASI™ RPR card test for syphilis. Arlington Scientific (USA). 2014.
- Serodia TP-PA® passive particle agglutination test for detection of antibodies to Treponemal pallidum. NHANES. 2001.
- Bukh J. The history of Hepatitis C Virus (HCV): Basic research reveals unique features in phylogeny, evolution and the viral life cycle with new perspectives for epidemic control. J hepatol. 2016; 65(1): S2-S21.
[Crossref] [Google scholar] [Pubmed]
- Esposito I, Marciano S, Haddad L, Galdame O, Franco A, Gadano A, et al. Prevalence and factors related to natural resistance-associated substitutions to direct-acting antivirals in patients with genotype 1 hepatitis C virus infection. Viruses. 2018; 11(1): 3.
- Ufearo H, Kambal K, Onojobi GO, Nouraie M, Agbemabiese C, Diaz S, et al. Complete blood count, measures of iron status and inflammatory markers in inner-city African Americans with undiagnosed hepatitis C seropositivity. Clin Chim Acta. 2010; 411(9-10): 653-656.
[Crossref] [Google scholar] [Pubmed]
- Jewett A, Al-Tayyib AA, Ginnett L, Smith BD. Successful integration of hepatitis C virus point‐of‐care tests into the Denver metro health clinic. AIDS Res Treat. 2013; 2013(1): 528904.
[Crossref] [Google scholar] [Pubmed]
- Randall G, Grakoui A, Rice CM. Clearance of replicating hepatitis C virus replicon RNAs in cell culture by small interfering RNAs. Proc Natl Acad Sci. 2003; 100(1): 235-240.
[Crossref] [Google scholar] [Pubmed]
- Sarkar M, Bacchetti P, Tien P, Mileti E, French AL, Edlin BR, et al. Racial/ethnic differences in spontaneous HCV clearance in HIV infected and uninfected women. Dig Dis Sci. 2013; 58: 1341-1348.
[Crossref] [Google scholar] [Pubmed]
Author Info
Cynthia Turner1,2*, Tuan Phan2, OsaroMgbere1, Jennifer Perez1 and Lupita Thornton12Department of Health, Texas Southern University, Houston, Texas, USA
Received: 22-Mar-2024 Accepted: 08-Apr-2024 Published: 15-Apr-2024, DOI: 10.31858/0975-8453.15.4.146-152
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3