Research Article - (2022) Volume 13, Issue 9
Injury Protection Strategies for H63D Syndrome Patients Suffering from Cataplexy
Carolina Diamandis1*, Jacob S Adams2, David Seideman1, Riku Honda2 and Lucas Smith1,2Abstract
Patients suffering from H63D syndrome have a significant incidence of narcolepsy with cataplexy as a symptom. Previous studies have shown that the presence of narcolepsy with cataplexy in the context of H63D syndrome is a surrogate marker for structural brain damage. Now, the aim was to clarify which measures best protect affected patients with cataplexy from injury. Our study suggests that every patient with cataplexy and corresponding risk of injury from falls and similar consequences of seizures with more than two high-risk incidences per month should be prescribed a standard wheelchair with restraining elements, which should be used permanently without any exception.
Keywords
Cataplexy, Narcolepsy, H63D syndrome
Introduction
H63D syndrome and cataplexy
Cataplexies are the most specific symptom of narcolepsy type 1 and therefore it’s most important clinical diagnostic sign. It is a loss of tone of the striated muscles, usually in the legs, arms, hands, and neck/facial muscles (Pizza F, et al., 2018; Moturi S and deWolfe JL, 2010). Eye coordination and speech may also be affected. The duration of the loss of tone in cataplexy is short, usually a few seconds, and longer than one to three hours in only about 10%-20% of cases (Hartse KM, et al., 1988; Morgenthaler TI, et al., 2007). As we were able to show in earlier studies narcolepsy with cataplexy is a cardinal symptom of progressed H63D syndrome which correlates with findings consistent with brain damage in transcranial sonography (hyper-echogenicity in the substantia nigra and abnormal findings in parts of the basal ganglia) as to be seen in Figure 1 below. Interestingly, in H63D syndrome patients, the intensity of active motor disturbances (eg: Tics, hyperkinesias) gradually decreases once narcolepsy with cataplexy occurs (Reading P, 2019; Matos N, et al., 2017). This is usually seen in the fourth and fifth decades of life and correlates strongly with the progression of irreversible damage to the substantia nigra and parts of the basal ganglia. The narcoleptic and cataplectic symptomatology can take on massive progressive forms in H63D syndrome (Figure 1) (Diamandis C and Tudor A, 2021; Diamandis C, et al., 2021).
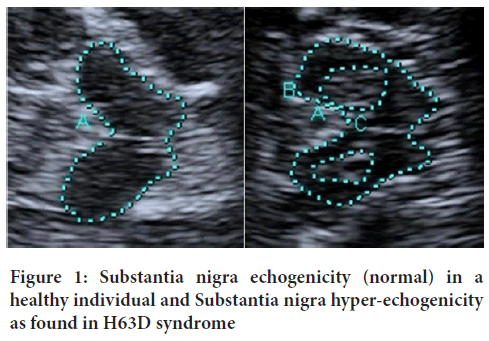
Figure 1: Substantia nigra echogenicity (normal) in a healthy individual and Substantia nigra hyper-echogenicity as found in H63D syndrome
Cataplectic seizures are associated with a significant risk of injury as is also known from other conditions with seizures (Camfield C and Camfield P, 2015). However, in the case of cataplexies more severe injuries (eg: Broken bones) seem to occur more often. We speculate that this effect is explainable in the lower grade of institutionalization of patients with H63D associated narcolepsy with cataplexy. How this problem can be minimized most effectively in addition to pharmaceutical treatment was investigated independently by two clinics in the Middle East and India that are affiliated with the H63D Syndrome Research Consortium. The results were made available to the Consortium in anonymized form. The fact that the risk of injury due to cataplexy is not taken as seriously as in the case of other neurological seizure disorders remains an unanswered question (Adams R and Mayhew IG, 1985; Peacock J and Benca RM, 2010; Pillen S, et al., 2017; Jory C, et al., 2019; Trefler E, et al., 2004; Diamandis C and Tudor A, 2021; Diamandis C, et al., 2021; Deekollu D, et al., 2005).
Materials and Methods
Two hundred patients with relevant cataplexy seizures, defined as more than 2 seizures with falls and/or injuries and/or or property damage, aged 24 to 49 years, average age 32 (169 male, 31 female, no significant sex difference in results) were asked by means of structured questionnaires about their seizures and their consequences in the 12 months preceding the study. Depending on the type and focus of the cataplectic seizures, the patients were then given medical aids. These were to be worn/used for one year. Compliance and relevant events were reviewed and queried in a structured manner on a monthly basis.
Results
Results of the initial survey
In our patient collective 198 out of 200 individual had at least one relevant injury connected to a cataplectic seizure to report (eg: With significant scars) 185 out of 200 more relevant injuries (eg: broken bones) (Table 1) (Camfield C and Camfield P, 2015; Wirrell EC, 2006; Frey K, et al., 2020).
| Cataplectic seizures | Average values |
|---|---|
| Risky cataplectic episodes in average per months | 72 |
| Number of cataplectic seizures with major injuries | 11 |
| Number of cataplectic seizures with relevant injuries | 39 |
| Number of cataplectic seizures per month which needed medical attention | 12 |
Table 1: Below results are average values per patient (related to a defined month)
Medical aids provided
The type of medical aid was prescribed according to the cataplexy patterns most typical for the individual affected (Table 2).
| Medical aid | Average values |
|---|---|
| Orthoses (limited movement model) for both arms | 14 |
| Orthoses (no movement model, cast like) for both arms | 12 |
| Stabilizing leg braces for both legs (limited knee movement) | 24 |
| Teeth protector without a stabilizing brace | 8 |
| Teeth protector with a stabilizing brace | 4 |
| Crutches | 24 |
| Epilepsy helmet with chin and face protection | 64 |
| Normal wheelchair | 32 |
| Wheelchair with stabilizing components | 18 |
Table 2: Type of medical aid was prescribed according to the cataplexy patterns most typical for the individual affected
Results after one year
Remarkably, no subjects dropped out and compliance was unexpectedly good. Only about one third of those patients who were assigned a wheelchair and half of those with a protective helmet needed some interventions in the first weeks to actually use the wheelchair all day (despite being able to walk) respectively to get rid of the shame regarding the helmet. At the same time, all subjects for whom this was indicated received thrombosis prophylaxis and regular physiotherapy with physical training to counteract muscle loss. This worked without any problems, presumably also because the patients had been informed comprehensively and calmly beforehand (Table 3).
| Medical aid | Percentage |
|---|---|
| Orthoses (limited movement model) for both arms | -61% |
| Orthoses (no movement model, cast like) for both arms | -72% |
| Stabilizing leg braces for both legs (limited knee movement) | -34% |
| Teeth protector without a stabilizing brace | -10% |
| Teeth protector with a stabilizing brace | -12% |
| Crutches | No significant effect |
| Epilepsy helmet with chin and face protection | -69% |
| Normal wheelchair | -91% |
| Wheelchair with stabilizing components | -98% |
Table 3: Change in injuries or dangerous events, according to the medical aid used
Psychological effects
Medical aids, especially restrictive ones, can also have a psychological effect. Thus, it was also necessary to examine the extent to which the individual aids caused psychological stress for the patients. This was recorded on a self-assessment scale from 0 (no burden) to 10 (severe emotional distress), at the time points of 1 month, 6 months and 12 months (Table 4).
| Medical aid | Month 1 | Month 6 | Month 12 |
|---|---|---|---|
| Orthoses (limited movement) both arms | 2 | 2 | 1 |
| Orthoses (cast like) for both arms | 5 | 3 | 1 |
| Stabilizing leg braces | 3 | 1 | 2 |
| Teeth protector | 7 | 7 | 6 |
| Teeth protector with a stabilizing brace | 9 | 7 | 7 |
| Crutches | 1 | 1 | 0 |
| Epilepsy helmet head, chin and face | 6 | 5 | 2 |
| Normal wheelchair | 8 | 3 | 1 |
| Wheelchair with stabilizing components | 9 | 6 | 2 |
Table 4: Self-assessment scale from 0 (no burden) to 10 (severe emotional distress), at the time points of 1 month, 6 months and 12 months
Discussion
The highly significant results were surprising even for the physicians involved. The use of wheelchairs proved to be particularly effective, while the use of rigid whole-arm orthoses with fixation at 80 degrees, including stiffening of the wrists, was somewhat less effective but also highly significant and helpful.
However, it is contrary to the intuition of every physician to immobilize healthy limbs with medical devices or to permanently immobilize people in a wheelchair who would be able to walk, even if the muscles are preserved with guided training. Nevertheless, one cannot argue away the risks due to cataplectic seizures. Putative concerns about the patient’s well-being (eg: Fear of stigmatization or mobility in daily life) are soft factors that should not be a contraindication (Peacock J and Benca RM, 2010; Pillen S, et al., 2017; Jory C, et al., 2019; Trefler E, et al., 2004; Laplante MP and Center DS, 2003; Simpson RC, et al., 2008; Chang ET, et al., 2020; Diamandis C and Tudor A, 2021; Diamandis C, et al., 2021; Deekollu D, et al., 2005; Camfield C and Camfield P, 2015; Frey K, et al., 2020).
A good half of the wheelchair users even had stronger leg and back muscles after a year in their wheelchairs, without any walking, thanks to supervised physiotherapy. Moving around in the wheelchair also strengthened the arm and shoulder muscles in the classic models. The protective effect, on the other hand, was better in those wheelchairs that had fixation elements, so that these represent the gold standard in injury prevention for patients with cataplexy. The only minor injury in the group of patients who used a wheelchair with stabilizing components was during transfer from wheelchair to bed. Since getting around in a wheelchair with fixating and/or stabilizing components makes moving by muscle power almost impossible, models with electric motors are to be preferred in this case. However, since these are considerably more expensive and significantly restrict mobility in numerous situations during daily use, standard wheelchairs with minor fixating features are good compromise solutions.
Protective helmets alone were not sufficiently effective, which is consistent with earlier results from another study group (Deekollu D, et al., 2005). However, also non-flexible arm orthoses (similar to a full arm cast) were more helpful than expected. If a patient refuses to accept a wheelchair despite detailed explanations, arm orthoses of this type are a possible alternative, especially together with a helmet protecting the head and face. The psychological effects (Jory C, et al., 2019; Trefler E, et al., 2004) are acceptable, which was confirmed by the fact that none of the subjects dropped out of this study.
Conclusion
Our study suggests that every patient with cataplexy and corresponding risk of injury from falls and similar consequences of seizures with more than two high-risk incidences per month should be prescribed a standard wheelchair with restraining elements, which should be used permanently without any exception. This stands in contrast to the recommendations in the case of epilepsy, since in that disease fixation can have unfavorable consequences during seizures. It seems to be reasonable to prevent muscleloss in the back and hip area with specific training for the patients who have to use a wheelchair due to cataplexies. A healthy back is important and should be maintained. However, if medical leg training should be paid for by insurances is questionable since the patients will be bound to their wheelchair for as long as they suffer from cataplexies, and that is normally for life. Therefore, it could be argued that muscle atrophy in the legs is an acceptable side effect of wheelchair use and does not require therapy, but actually improves compliance. Furthermore, a wheelchair can only fully develop its protective effects if it is used permanently, professionally (eg: During transfers from wheelchair to bed), and without interruptions. Based on our results, the prescription of wheelchairs with safety elements should be part of the standard care for people with moderate to severe cataplexy in the context of H63D syndrome.
Ethical Standards and Patient’s Rights
All patients gave their informed consent, their health and safety was not endangered and the authors of this study got all results in an anonymized form. The supervision bodies were the relevant administrations responsible for the location where the data was generated. Full compliance with the latest version of the Declaration of Helsinki was ensured at all times.
References
- Pizza F, Antelmi E, Vandi S, Meletti S, Erro R, Baumann CR, et al. The distinguishing motor features of cataplexy: A study from video-recorded attacks. Sleep. 2018; 41(5): 26.
[Crossref] [Google Scholar] [Pubmed]
- Moturi S, DeWolfe JL. Isolated Cataplexy. Sleep Review. 2010.
- Hartse KM, Zorick FJ, Sicklesteel JM, Roth T. Isolated cataplexy: A familial study. Henry Ford Hosp Med J. 1988; 36(1): 24-27.
[Google Scholar] [Pubmed]
- Morgenthaler TI, Kapur VK, Brown T, Swick TJ, Alessi C, Aurora RN, et al. Practice parameters for the treatment of narcolepsy and other hypersomnias of central origin. Sleep. 2007; 30(12): 1705-1711.
[Crossref] [Google Scholar] [Pubmed]
- Reading P. Cataplexy. Pract Neurol. 2019; 19(1): 21-27.
[Crossref] [Google Scholar] [Pubmed]
- Matos N, Gaig C, Santamaria J, Iranzo A. Cataplexy causing subdural hematomas. Sleep Med. 2017; 100(30): 15-16.
[Crossref] [Google Scholar] [Pubmed]
- Diamandis C, Tudor A. Medical devices that should be prescribed to patients with cataplexy to reduce their risk of injury. Authorea Preprints. 2021.
- Diamandis C, Adams JS, Honda R, Lazar M, Seideman D. Regularly missed symptoms in primary and secondary narcolepsy. Authorea Preprints. 2021.
- Camfield C, Camfield P. Injuries from seizures are a serious, persistent problem in childhood onset epilepsy: A population-based study. Seizure. 2015; 27: 80-83.
[Crossref] [Google Scholar] [Pubmed]
- Adams R, Mayhew IG. Neurologic diseases. Vet Clin North Am Equine Pract. 1985; 1(1): 209-234.
[Crossref] [Google Scholar] [Pubmed]
- Peacock J, Benca RM. Narcolepsy: Clinical features, co-morbidities and treatment. Indian J Med Res. 2010; 131(2): 338.
[Google Scholar] [Pubmed]
- Pillen S, Pizza F, Dhondt K, Scammell TE, Overeem S. Cataplexy and its mimics: Clinical recognition and management. Curr Treat Options Neurol. 2017; 19(6): 1-20.
[Crossref] [Google Scholar] [Pubmed]
- Jory C, Oak K, Organ C, Mclean B, Shankar R. Head first: Review of epilepsy head injury risk and protection. Seizure. 2019; 71:66-79.
[Crossref] [Google Scholar] [Pubmed]
- Trefler E, Fitzgerald SG, Hobson DA, Bursick T, Joseph R. Outcomes of wheelchair systems intervention with residents of long-term care facilities. Assist Technol. 2004; 16(1): 18-27.
[Crossref] [Google Scholar] [Pubmed]
- Deekollu D, Besag FM, Aylett SE. Seizure-related injuries in a group of young people with epilepsy wearing protective helmets: Incidence, types and circumstances. Seizure. 2005; 14(5): 347-353.
[Crossref] [Google Scholar] [Pubmed]
- Wirrell EC. Epilepsy‐related injuries. Epilepsia. 2006; 47: 79-86.
[Crossref] [Google Scholar] [Pubmed]
- Frey K, Zöllner JP, Knake S, Oganian Y, Kay L, Mahr K, et al. Risk incidence of fractures and injuries: A multicenter video-EEG study of 626 generalized convulsive seizures. J Neurol. 2020; 267(12): 3632-3642.
[Crossref] [Google Scholar] [Pubmed]
- Laplante MP, Center DS. Demographics of wheeled mobility device users. Conference on space requirements for wheeled mobility. 2003.
- Simpson RC, Lopresti EF, Cooper RA. How many people would benefit from a smart wheelchair? J Rehabil Res Dev. 2008; 45(1).
[Crossref] [Google Scholar] [Pubmed]
- Chang ET, Lin CL, Chen SF, Hsu CY, Shen YC. Risk of bone fractures in patients with narcolepsy: A nationwide population-based cohort study. Sleep Med. 2020; 70: 55-59.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Carolina Diamandis1*, Jacob S Adams2, David Seideman1, Riku Honda2 and Lucas Smith1,22Department of Medical Sciences, International H63D Consortium, Rare Diseases Research Consortium, Kifissias, Greece
Citation: Diamandis C: Injury Protection Strategies for H63D Syndrome Patients Suffering from Cataplexy
Received: 29-Aug-2022 Accepted: 23-Sep-2022 Published: 30-Sep-2022, DOI: 10.31858/0975-8453.13.9.577-580
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






