Research Article - (2023) Volume 14, Issue 11
Outcomes of Coronary Endarterectomy in Patients Undergoing Coronary Artery Bypass Grafting for Coronary Artery Disease: A Retrospective Study
Aakash Dinesh Joshi*, Prashant Harsur and Vivek PillaiAbstract
Complete revascularization of coronary arteries, and mainly of the Left Anterior Descending artery (LAD) which plays a significant role in terms of postoperative outcomes, is the primary objective in Coronary Artery Bypass Grafting (CABG). Nowadays, more and more patients having stenosis in one or two coronary vessels tend to be treated by Percutaneous Coronary Intervention (PCI). As a result, diffuse Coronary Artery Disease (CAD) is more likely among patients referred for CABG. However, up to 25% of patients with diffuse CAD cannot be safely and successfully treated by standard CABG. Therefore, several techniques including Coronary Endarterectomy (CE), which involves the removal of the atherosclerotic core from the coronary artery lumen through an arteriotomy, have been proposed to expand surgical possibilities.
Total of 62 patients underwent coronary artery bypass grafting with coronary endarterectomy. 62 patients fulfilled inclusion our study and were followed up. Out of 62, more than half of patients had four grafts (51.6%), followed by five grafts (27.4%), three grafts in 16.1% of patients and six graft in 3.2% of patients. Out of total patients 32 (51.6%) patients had 3 venous grafts, followed by 17 (27.4%) patients had 4 venous grafts, 10 (16.1%) patient had 2 venous graft and one patient (1%) with one venous graft in our study.
In our study, we used Left Internal Mammary Artery (LIMA) to anastomosed with LAD in 60 patients which constitutes 96.8%, 11 patients had only right coronary artery bypass grafting with 1.6% of patients, LAD+Right Coronary Artery (RCA)+Posterior Descending Artery (PDA). Additionally LAD+RCA were territory was grafted in one patient. Out of 62 patients, LAD was endarterectomized in 15 patients and 24.2% and endarterectomy for PDA artery was done in 7 patients (11.3), followed by second Obtuse Marginal (OM-2) in 4 patients (6.5%), first Obtuse Marginal (OM-1) in 2 patients (3.2%), OM-3 in 1 patient (1.6%) and lastly distal RCA in 1 patient (1.6%). Total mortality till date was 5 (8.06%) and 1 in hospital mortality due to multi-organ dysfunction syndrome out of total 62 patients.
In the recent decades, the treatment of older patients with diffuse CAD, alongside multiple comorbidities and high expectations for successful treatment, has become a real challenge. CE is a surgical method that can provide acceptably effective and safe results in the treatment of CAD. CE as an adjunct to CABG has a significant role in achieving adequate revascularisation and in improvement of long term outcomes.
Keywords
Endarterectomy, Coronary Artery Disease (CAD), Left Anterior Descending artery (LAD), Percutaneous Coronary Intervention (PCI)
Introduction
Coronary Artery Bypass Grafting (CABG) aims to completely revascularize coronary arteries, especially the LAD, which affects postoperative results. In the present day, there is a growing trend towards the utilisation of Percutaneous Coronary Intervention (PCI) as a treatment approach for patients presenting with stenosis in either one or two coronary vessels (Takanashi S, et al., 2008). Consequently, patients who are referred for Coronary Artery Bypass Grafting (CABG) are at an increased likelihood of having diffused Coronary Artery Disease (CAD) (Filsoufi F, et al., 2007; ElBardissi AW, et al., 2009). Nevertheless, a significant proportion of individuals diagnosed with diffuse Coronary Artery Disease (CAD) are unable to undergo conventional Coronary Artery Bypass Grafting (CABG) due to safety concerns and the limited likelihood of successful outcomes (Santini F, et al., 2002). Several methods have been proposed to increase the range of surgical options, one of which is coronary endarterectomy, which involves the arteriotomy-based removal of the atherosclerotic core from the coronary artery lumen. While contrasting open and closed endarterectomy, the former is preferable (Fundaro P, et al., 1987). The perioperative death rate was lower among patients who underwent open endarterectomy, but the difference was not statistically significant. However, this subset was linked to markedly better long-term outcomes than the rest. Five-year survival rates for open and closed endarterectomy were, respectively, 90.7% and 74%. Furthermore, 85.2% of patients who underwent open endarterectomise did not suffer from angina or congestive heart failure throughout the follow-up period, compared to 76.6% of patients who underwent closed endarterectomise (Nishi H, et al., 2005). As a result, the open approach is the best method of endarterectomy, while being time-consuming. In order to better understand the long-term effects of coronary endarterectomy on patients with coronary artery disease, the current retrospective observational study was conducted. The purpose of this research was to document the occurrence of serious cardiac and cerebrovascular complications following coronary endarterectomy and coronary artery bypass grafting.
Standard intraoperative monitoring procedures and a Cardiopulmonary Bypass (CPB) circuit were used. All incisions were made along the median line of the sternum. Heparin was administered to maintain an active clotting time more than 400 seconds during conduit harvesting (internal mammary artery, saphenous vein, and rarely radial artery). Although suction-type mechanical stabilizers were utilized to hold the target coronary artery in place during grafting, the on-pump CABG approach was the standard in the vast majority of cases. Cardiopulmonary Bypass (CPB) was started through the conventional method of aorta-right atrial cannulation. The decision to endarterectomise a vessel was made preoperatively when a localized lesion blocked a sufficient distal stream (i.e. complete occlusion), distal diffuse lesion, multi-segment lesion, or when a calcified or extremely thick plaque burst, making anastomosis troublesome or hindering the stream. Coronary endarterectomise were performed manually by gradual steady and continuous traction of atheromatous plaque using Ring Forceps, right-angled artery forceps, and closed procedures, and were then reconstructed using a pre-planned graft. Arteriotomy incisions were typically 8-10 mm long, but could be lengthened by additional 5 mm if necessary to clear the artery of all plaque. An extremely sensitive ring forceps/coronary artery endarterectomy dissector was utilized to create a plane between the media and the atherosclerotic plaque (Figure 1). Slow steady and constant traction, aided by another ring forceps (counter traction), were attempted to remove the plaque, and succeeded in removing the largest piece of plaque. The distal piece was carefully expelled because of the risk of proximal dissection and the possibility of occlusion from a big septal branch, oblique branches, or even the circumflex artery. To finish the distal anastomosis, the surgeon would lengthen the arteriotomy incision; occasionally, a venous patch would be utilized instead. To ensure successful removal, the atheromatous plaque was carefully inspected for a tapered end (Figure 2). The reassuring backflow of blood from the distal conduit following atheroma removal is another feature unique to on-pump CABG endarterectomy. The intensive care unit provided round-the-clock monitoring and care for all of the patients. Heparin bridging to warfarin was used to manage the patient from the first day after surgery to the next three to six months. Aspirin, 150 mg od, was administered to prevent acute thrombosis in the graft and the endarterectomized artery. Patients were typically started on 3 mg of warfarin daily for the first 2 post-operative days, then reduced to 2/1 mg for the remaining 3 to 6 months as our regional goal International Normalized Ratio (INR) was 1.5-2.0.

Figure 1: Sensitive ring forceps/coronary artery endarterectomy dissector to create a plane between the media and the atherosclerotic plaque
Figure 2: Instruments used for the removal of the atheromatous plaque during coronary artery bypass grafting
Materials and Methods
This study was approved by the Institutional Ethical Board of Sree Chitra Tirunal Institute of Medical Science and Technology (SCTIMST). Permission to used computer recorded data for conduction of study was obtained by the head of department of Cardio-thoracic Department of SCTIMST. Patient who underwent above mentioned operative during the period of 01/01/2000 to 31/12/2010 were included in the study. Patients who under went any other concomitant procedures such as carotid endarterectomy, Valve repair or replacement along with Coronary Artery Bypass Grafting (CABG) were excluded. 62 cases were participated in this study who has given consent to the participation. Secondary data were recorded by principal investigator after going through medical records. All the patients underwent follow up after the procedure and routinely as per departmental protocol. Follow up involved transthoracic Echocardiogram (ECHO), Electrocardiogram (ECG), Chest X-ray and International Normalized Ratio (INR) monitoring. Patients who were lost to follow up were contacted through Telephonic interview. Patients were asked about symptoms in the follow up period.
Statistical analysis using International Business Machines (IBM) Statistical Package for Social Science (Statistics for windows, version 21.0, Armonk, NY: IBM corp.) was done and the comparison of data was carried out by applying statistical tests in order to find statistical significance of the results. P value of <0.05 was considered as statistically significant. Kaplan Meier curve is used to assess the survival rate of conducted surgery.
Results
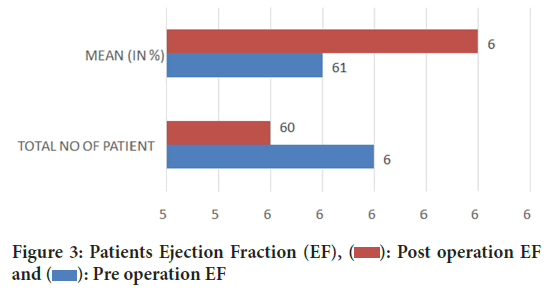
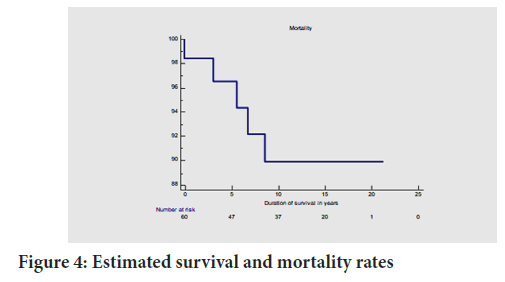
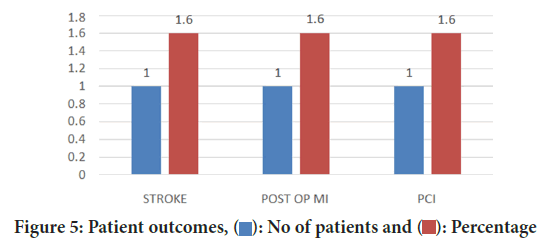
A single patient only underwent surgery of on-pump CABG. The mean age at surgery was 68.5 ± 8 years. The mean cross clamp time was 73.3 ± 31.8 minutes, and cardiopulmonary bypass time was 119 ± 40.9 minutes. Mean ventilation hour were 15 ± 2.9 hours. Mean hospital stay was 10.5 ± 4.8 days and mean Intensive Care Unit (ICU) stay was 5.3 ± 2.9 days in our study (Table 1). Out of these patients the highest that is 92% (n=57) were male and only 8% (n=5) were the females. Among all the patients, existing co-morbidity showed as 64.5% (n=40) patients had diabetes. Following this 37% (n=37.1) patients had hypertension and 24% (n=24.2) patients had dyslipidemia. Among those 34% (n=21) had adverse habit of smoking. 96.8% (n=60) of patients had triple vessel disease. More than half patients had 4 grafts (Table 2). Pre-operative ejection fraction is reduced by two in post-operative measures (Figure 3). 60 patients received left internal mam-mary artery anastomosis to LAD, 2 patients has only venous graft as conduits. The most common vessel to undergo endarterectomy was RCA, 31 patients (50%). Endarterectomy of LAD was done in 15 (24.2%) patients PDA artery was done in 7 patients (11.3%), followed by OM-2 in 4 patients (6.5%), OM-1 in 2 patients (3.2%), OM-3 in 1 patient (1.6%) (Table 3) and total mortality is 5. The estimated 1 year survival is 98.45%, 5 year survival was 96.5% and 10 year survival was 89.9 % (Figure 4). One patient had stroke, another patient had acute myocardial infarction after 2 years of surgery for which PCI was done. There were no re-operations (Figure 5).
| Variables | Mean | Standard deviation |
|---|---|---|
| Age (years) | 68.5 year | ± 8 years |
| Cross clamp time (minutes) | 73.3 ± 31.8 minutes | ± 31.8 minutes |
| CPB (time) | 119.2 ± minutes | ± 40.9 minutes |
| Ventilation hours | 15 ± 2.9 hours | ± 2.9 hours |
| Hospital stay (days) | 10.5 ± 4.8 days | ± 4.8 days |
| ICU stay (days) | 5.3 ± 2.9 days | ± 2.9 days |
Table 1: Different pathological parameters of the patients
| Parameter | No. of participants | Percentage (%) |
|---|---|---|
| Male | 57 | 91.9 |
| Female | 5 | 8.1 |
| Diabetes | 40 | 64.5 |
| Hypertension | 23 | 37.1 |
| Dyslipidemia | 15 | 24.2 |
| Smoking | 21 | 33.9 |
| Triple vessel disease | 60 | 96.8 |
| 4 grafts | 32 | 51.60 |
Table 2: General characteristics of the patients
| Vessel endarterectomized | No of patients | Percentage (%) |
|---|---|---|
| LAD | 15 | 24.2 |
| Diagonal one | 2 | 3.2. |
| OM-1 | 2 | 3.2 |
| OM-2 | 4 | 6.5 |
| OM-3 | 1 | 1.6 |
| RCA | 31 | 50 |
| PDA | 7 | 11.3 |
Table 3: Different vessels which underwent endarterectomized
Figure 3: Patients Ejection Fraction (EF),  : Post operation EF
and
: Post operation EF
and  : Pre operation EF
: Pre operation EF
Figure 4: Estimated survival and mortality rates
Figure 5: Patient outcomes,  : No of patients and
: No of patients and  : Percentage
: Percentage
Discussion
It stands to reason that the greater the number of endarterectomized vessels, the greater the risk of catastrophic complications including MI and death during and after surgery (Keogh BE, et al., 1991). The technique can be done successfully and securely with or without cardiopulmonary bypass. Soylu E, et al., 2014 found no statistically significant difference in perioperative morbidity and mortality or long-term outcomes between patients who underwent onor off-pump CE. The potential risks of the operation need to be discussed now. The most serious issue that can arise with CE is a perioperative MI. Based on the data we gathered, we found that the risk of in-hospital death among our patients ranged from 0% to 1% in the days following surgery. Stroke is another life-threatening condition. Stroke occurred in 1% of our patients, which is equivalent to the 3%.
Between 0% and 19%, surgical mortality was seen. There was no statistically significant difference between patients who had on-pump or offpump CABG, regardless of whether the procedure was conducted using an open or closed approach. Soylu E, et al., 2014 found that individuals who had CE had a higher risk of MI and death than those who got CABG alone. The authors did clarify, though, that there was scant evidence to back up this claim because of the substantial heterogeneity among the included research. To date, we have had 5 patients who have passed away while hospitalised (1.6%). Consistent with prior research, we found that LAD endarterectomy and endarterectomy of multiple coronary arteries contributed significantly to the early death rate in the ICU among patients in the highrisk category (Schmitto JD, et al., 2009). Early mortality after Coronary Artery Bypass Grafting (CABG) ranges from 2% to 15%. Few researchers reported no deaths within 30 days after CABG with CE in their small series investigation, but Naseri E, et al., 2003, compared on-pump and off-pump CABG with CE and reported a 2.2% mortality rate in a cohort of 44 patients. Survival rates after CE with CABG have been studied previously; those published by Eryilmaz S, et al., 2003 reveal no mortality at one year follow-up in their small group study, while those published by Vohra HA, et al., 2006, observe survival rates of 91.5% at 1 year and 87.9% at 5 years, which are similar to our findings. There was a 98.4% one-year survival rate, 96.5% five-year survival rate, and 81.4% ten-year survival rate.
Conclusion
The management of older patients with diffuse CAD has grown increasingly difficult in recent decades due to the presence of many coexisting conditions and high expectations for treatment success. When it comes to treating CAD, CE is a surgical option that has shown to be both successful and safe. When used with CABG, CE can greatly aid in revascularization and enhance long-term results.
As the study is retrospective lapses in data recoding can produce error in the results. Also Echocardiography parameters may vary between observers producing a confounding factor in the study. The above study excluded patients who underwent concomitant procedures.
References
- Takanashi S, Fukui T, Miyamoto Y. Coronary endarterectomy in the left anterior descending artery. J Cardiol. 2008; 52(3): 261-268.
[Crossref] [Google Scholar] [Pubmed]
- Filsoufi F, Rahmanian PB, Castillo JG, Chikwe J, Adams DH. Excellent results of contemporary coronary artery bypass grafting with systematic application of modern perioperative strategies. Heart Surg Forum. 2007; 10(5): E349-E356.
[Crossref] [Google Scholar] [Pubmed]
- ElBardissi AW, Balaguer JM, Byrne JG, Aranki SA. Surgical therapy for complex coronary artery disease. Semin Thorac Cardiovasc Surg. 2009; 21(3): 199-206.
[Crossref] [Google Scholar] [Pubmed]
- Santini F, Casali G, Lusini M, D'Onofrio A, Barbieri E, Rigatelli G, et al. Mid-term results after extensive vein patch reconstruction and internal mammary grafting of the diffusely diseased left anterior descending coronary artery. Eur J Cardiothorac Surg. 2002; 21(6): 1020-1025.
[Crossref] [Google Scholar] [Pubmed]
- Fundaro P, di Biasi P, Santoli C. Coronary endarterectomy combined with vein patch reconstruction and internal mammary artery grafting: experience with 18 patients. Tex Heart Inst J. 1987; 14(4): 389-394.
[Google Scholar] [Pubmed]
- Nishi H, Miyamoto S, Takanashi S, Minamimura H, Ishikawa T, Kato Y, et al. Optimal method of coronary endarterectomy for diffusely diseased coronary arteries. Ann Thorac Surg. 2005; 79(3): 846-852.
[Crossref] [Google Scholar] [Pubmed]
- Keogh BE, Bidstrup BP, Taylor KM, Sapsford RN. Angioscopic evaluation of intravascular morphology after coronary endarterectomy. Ann Thorac Surg. 1991; 52(4): 766-772.
[Crossref] [Google Scholar] [Pubmed]
- Soylu E, Harling L, Ashrafian H, Athanasiou T. Does coronary endarterectomy technique affect surgical outcome when combined with coronary artery bypass grafting?. Interact Cardiovasc Thorac Surg. 2014; 19(5): 848-855.
[Crossref] [Google Scholar] [Pubmed]
- Schmitto JD, Kolat P, Ortmann P, Popov AF, Coskun KO, Friedrich M, et al. Early results of coronary artery bypass grafting with coronary endarterectomy for severe coronary artery disease. J Cardiothorac Surg. 2009; 4: 1-7.
[Crossref] [Google Scholar] [Pubmed]
- Naseri E, Sevinç M, Erk MK. Comparison of off-pump and conventional coronary endarterectomy. Heart Surg Forum. 2003; 6(4): 216-219.
[Google Scholar] [Pubmed]
- Eryilmaz S, Inan MB, Eren NT, Yazicioglu L, Corapcioğlu T, Akalin H. Coronary endarterectomy with off-pump coronary artery bypass surgery. Ann Thorac Surg. 2003; 75(3): 865-869.
[Crossref] [Google Scholar] [Pubmed]
- Vohra HA, Kanwar R, Khan T, Dimitri WR. Early and late outcome after off-pump coronary artery bypass graft surgery with coronary endarterectomy: A single-center 10-year experience. Ann Thorac Surg. 2006; 81(5): 1691-1696.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Aakash Dinesh Joshi*, Prashant Harsur and Vivek PillaiCitation: Joshi AD: Outcomes of Coronary Endarterectomy in Patients Undergoing Coronary Artery Bypass Grafting for Coronary Artery Disease: A Retrospective Study
Received: 03-Oct-2023 Accepted: 25-Oct-2023 Published: 02-Nov-2023, DOI: 10.31858/0975-8453.14.11.706-709
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3