Research Article - (2023) Volume 14, Issue 4
Abstract
Allergy is the overreactions of the immune system to normally harmless substances. Globally, the percentage of people with allergies has shown an increasing trend, as well as the incidence of death caused by allergies, a symptom known as anaphylaxis. People with allergies have a harder life experience than normal people. However, unlike some common diseases that could be cured by medicines and human immune systems, allergy is incurable and can last for a lifelong time. With rising technologies and deeper understanding of the immune system and mechanisms of cells’ functions, many new types of medicines and therapies are being invented and improved in recent years. In this article, several existent medicine types and some potential treatment that might bring more options for allergic patients are discussed.
Keywords
Allergies, SARS-CoV-2, Vaccine
Introduction
For most people, when a friend gives you a peanut granola bar, you can eat it without hesitancy and feel just fine. However, for some, that same granola bar will produce a series of symptoms like skin becomes reddish, their throat becomes itchy, and eventually they faint. Why might someone eat a peanut product then pass over? The answer to this phenomenon is an inherited disorder called “allergy”. Allergy is the overreaction of the human immune system to external substances that are normally harmless to most people. When once affected individuals come in contact with an allergen, their body will react readily and develop a series of symptoms, including but not limited to sneezing, runny nose, watery eyes, etc. (Hirsch L, 2022).
External substances that cause allergic reactions are called allergy triggers, or allergens. Allergens include a variety of things-from airborne allergens (dust mites, pollens, molds and pets), food allergens (milk, egg, fish and peanuts) to insect stings, chemicals, and drugs (Hirsch L, 2022). For people with allergies, their lives are marked with caution; in order to prevent an allergic reaction, they may need to avoid eating certain foods or certain activities such as touching hairy animals. For those with dust or pollen allergies, they need to avoid outdoor activities especially in summer when these allergens are abundant outside, and in some cases, they need to take showers every day to remove allergens in their hair and keep the room clean to prevent remaining airborne allergens. Allergies can also lower an individual’s sleep quality. People with allergies are more likely to snore during sleep, which leads to other health problems (Rubinstein R, 2018). In addition, a survey based on 260 patients found a correlation between allergic rhinitis (a general term describing allergic reactions on the nose) and fatigue (Jaruvongvanich V, et al., 2016). Furthermore, some symptoms of allergy are specific to different allergens. Food allergies can cause scratchy feeling on face, swollen tongue and lips; hay fever (caused by airborne allergens) can lead to itching eyes and runny nose; insect allergies can lead to large swollen skins of the sting point (Hirsch L, 2022).
In contrast to pandemics or seasonal influenzas that may last months or years, allergies have accompanied the duration of recorded human history. The first case of food allergy was reported by Hippocrats about 2000 years ago, when he first identified different reactions among people toward dietary products (Heggie J, 2018). In 1819, hay fever was reported by Dr. John Bostock, and the branch of allergy study started in 1905 when Clemens von Pirquet described the relationship between the immune system and antigen and defined it as “allergy” (Heggie J, 2018). Immunotherapy research also started around the same time. The first antihistamine, known as pyrilamine, was discovered by Daniel Bovet in 1944 (Shampo MA and Kyle RA, 1999) and in 1948, corticosteroid therapy was found out to be helpful in treating patients with asthma and other allergic reactions (Charlotte Eye Ear Nose and Throat Associates, 2018; Benedek TG, 2011). With more allergy therapies available, people with different types of allergies can now be treated according to their individual situations.
Nonetheless, allergy is still a common disease affecting over 50 million Americans and accruing over 18 billion in annual cost for patients (ACAAI, 2021). In addition, individuals over age 4 share a similar likelihood of acquiring allergies regardless of their ages, gender, race, family income, parent education, and so forth (ACAAI, 2021). In the same time, a study found an increasing prevalence of asthmatic disorders in all age groups, and a higherthan-mean increase among 6-7 and 13-14 age groups (Asher MI, et al., 2006). With these statistics, it is important to pay attention to the large population basis of allergy patients.
Allergy acquisition
One mechanism of allergy acquisition is inheritance. The specific study on the genetic predisposition of having a certain inher ited study is called Genome-Wide Association Studies (GWAS Catalog, 2023). GWAS indicates the underlying biology basis of a phenotype, estimation of inheritance and risk chances, and helping the development of clinical medicines (Uffelmann E, et al., 2021). GWAS works by identifying associations between loci and traits that can cause diseases (GWAS Catalog, 2023). Loci (plural form of locus) is the physical location of a gene on a chromosome (Brookshire B, 2019). Later studies found other loci that are associated with certain problems. The 17q21 to the asthma phenotype and the 11q13 loci associated with allergic sensitization (Bønnelykke K, et al., 2015). Other following studies continued to discover more loci contributing to the allergy acquisitions and such findings support the role of gene involvement in allergy pathogenesis.
Meanwhile, environmental factors may also influence the acquisition of allergies. Though it does not directly cause someone to acquire allergies, certain environments may contribute to an individual’s increased sensitivity to allergens and symptom development. On a smaller scale, one’s living environment might put him or her at risk of developing allergy-related symptoms such as burning candles and incense sticks emits Volatile Organic Compounds (VOCs) that are capable of exacerbating symptoms of allergic rhinitis (Sanofi, 2019). On a broader scale, air pollutants also contribute to the development of allergic symptoms. Air pollutants might aggravate allergic reactions to alter one’s immunity and increase the severity of their symptoms (Jenerowicz D, et al., 2012). Limited studies discuss the relationship between the environment and direct acquisition of allergies, but other studies clearly showed a causal relationship between conditions of environment and development of allergic symptoms and sensitivities.
Introduction to anaphylaxis
Although allergy was first introduced in 1906, the term anaphylaxis wasn’t defined until 1902. At that time, French psychologist Chartles Richet found out the second exposure to marine animals’ toxins to dogs was lethal, after these dogs survived the first exposure to these toxins (Igea JM, 2013). Many subsequent health conditions correspond to different allergic symptoms, including hay fever (mainly runny nose and sneezing), allergic rhinitis (swollen, stiff joints from exposure of food allergens), hives (reddish, stinging skins), eczema (dry skin, itching), and especially anaphylaxis. Anaphylaxis is the most severe consequence of the allergic reaction and occurs within a few minutes after being exposed to allergens. Unlike symptoms of normal allergic reactions like airway itchiness, runny nose or swollen lips, without immediate care, one may fall into a coma and face life-threatening outcomes including death. Meanwhile, a patient under anaphylaxis may have difficulty breathing and a drop in blood pressure, leading to complications like brain damage, kidney failure, and heart attacks (Gotter A, 2019). However, having an allergy does not mean that anaphylaxis is inevitable, and in fact an improved estimation suggests that the frequency of anaphylaxis is about 50-2,000 episodes per 100,000 people; in other words, a life prevalence of 0.05% to 2% (Lieberman P, et al., 2006). The case fatality rate for anaphylaxis was between 0.25% to 0.33% among hospitalizations patients, about 63-99 deaths annually in the US (Borish L, et al., 2014). Due to the potential for severe complications, rapid and sudden stage development, and the large population of individuals with allergies, it is essential to develop medicines and measures that can save people under emergency situations.
Immune cascade of allergies
Allergy is an innate immune response where the body poses a general defense to allergens (John P, 2021). Our body has two types of immunity-
• Innate immunity
• Adaptive immunity
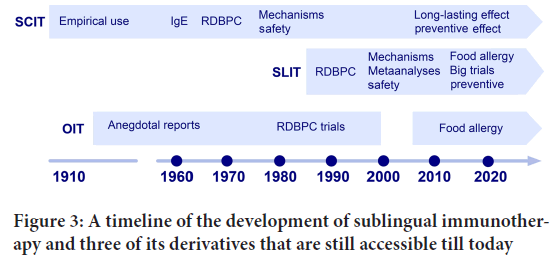
These include three lines of defense when exposed to allergens. The first line of defense is the superficial protection, skin, that blocks most pathogens from going into the body. Even if some allergens escape inside the body, the mucosal lining of nasal cavities and esophagus can secrete sticky fluid called mucus that captures pathogens and removes them from the body through spit or snot. At this line, our body protects us from general pathogens, which is the innate immunity. The second line of defense occurs at the cellular level where phagocytes, a type of immune cell, eliminate pathogens by eating them. At this stage, the body starts to dilate blood vessels to allow more white blood cells to travel to sites of allergen invasion and produces inflammation. Once the body is exposed to allergens, it will first trigger the Antigen Presenting Cells (APC), which is responsible for distinguishing the foreign substances from internal cells by breaking down the pathogen to many fragments of antigen, so the adaptive immune system can distinguish the pathogen (Learning) (Lumen, 2020). Then, T cells (or T lymphocytes, a type of white blood cell) will detect the signals of Antigen Presenting Cells (APCs) and trigger type 2 helper T cells (TH2) to produce chemicals (cytokines) to stimulate the B cell (part of the adaptive immune system), which in turn produce a type of antibody called immunoglobulin (IgE). These two lines are the adaptive immunity, meaning they pose defense against specific pathogens. When the person is exposed to allergens again, the IgE will bind to the mast cell and basophils, which will secrete histamine and other chemicals that trigger allergic reactions (Restak R, 2014). Usually, the whole process takes a few minutes to happen (Figure 1).
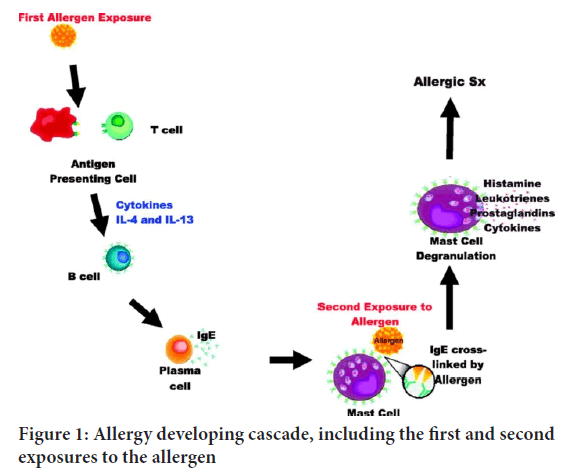
Figure 1: Allergy developing cascade, including the first and second exposures to the allergen
Materials and Methods
Current method: Epinephrine autoinjector/Epipen
The epipen was invented in 1980 to replace the previous epinephrine injector from World War II (WW2)-the Ana kit. Compared to the Ana kit where a prepared dose of epinephrine was set with a syringe and a needle, the EpiPen has the epinephrine syringe pre-loaded for emergency use (Bowden ME, 2021; Kaplan S, 2016). To use this device, the individual sticks the EpiPen into the skin of his or her outer thigh, waits until they hear a “click’” sound, and then removes the Epipen from the thigh. Epinephrine (also known as adrenaline) is a hormone naturally produced by the adrenal cortex above the kidneys; it helps relax the muscles and expand the airway (LibreTexts Biology, 2022). At the onset of an allergic reaction, the body expands the blood vessel pathways to allow more blood to flow, so the blood pressure suddenly drops. With one dose, the epinephrine goes into the thigh muscles and travels through blood vessels. Consequently, it boosts the heart-beat frequency and reduces the cytokine levels in the blood. Increasing the heart rate guarantees the normal blood flow in the body that prevents the person from permanent damage (like brain damage due to lack of oxygen); reducing the amount of chemicals helps alleviate the swelling of the body, thereby releasing symptoms like breathing difficulty and watery eyes (Sharma H, 2020). As one of the most accessible approaches to anaphylaxis, EpiPen has been a popular treatment since it was introduced to the public from 1987 when it was approved by FDA and about 3.6 million Americans were prescribed the Epipen in 2015 (Tunney K, 2016; Elenburg S and Blaiss MS, 2014). It sounds intriguing at first, and indeed it is the most successful treatment for anaphylaxis, but the primary problem is its price. The growing price makes it an unaffordable solution for many families; when the drug company Mylan began to sell Epipen in 2007, its price surged more than 400% and reached over $600 (Rubin R, 2016). Epipen is covered by many health insurances, yet the majority of the cost might still need to be undertaken by patients (Marsh T, 2019). Moreover, after the initial reaction, a person will need to be sent to the hospital for further observation, where the second reaction, or biphasic anaphyl axis, could happen. The biphasic anaphylaxis basically is the recurrence of anaphylaxis within 1-72 hours after the initial reaction; biphasic reaction has milder symptoms but still can be life-threatening (Morris SY, 2020).
Though the occurrence of biphasic reaction is low, a recent finding suggests that 1 in 4 (25%) patients will need further observation in the emergency room (Hamilton DK, 2019). If a biphasic reaction happens, a second dose of epinephrine is needed. Lastly, use of an Epipen cannot eradicate allergy, but rather gives a temporary relief, so it cannot be considered as a permanent solution.
Results and Discussion
Promising solution 1: CRISPR-based gene-editing
By artificially modifying an organism’s gene, gene editing has made many ground-breaking discoveries. It was first discovered by Francisco Mojica in 1993, when he was investigating how a group of microorganisms can survive in an environment with high salinity (an indicator of high concentration of salt). After sequencing these microorganisms’ DNA, Mojica found that there are repeating sequences next to each other. He coined the term SRSRs, abbreviation to “Short Regularly Spaced Repeats”. Later, he found similar patterns on other bacterium; by 2000, Mojica found CRISPR loci on 20 other different microbes, including Mycobacterium tuberculosis, Clostridium difficile and the plague bacteria Yersinia pestis (Lander ES, 2016). CRISPR stands for “Clustered Regularly Interspaced Short Palindromic Repeats”. With the discoveries like Cas 9 and tracrRNA, the type II (the one using Cas 9 protein as its effector) is one of the most effective ways in gene editing. CRISPR works by using a prepared guide RNA, or gRNA, to serve as the patch for the modified part, and then the gRNA part will attach to Cas 9 (CRISPR associated proteins). The gRNA will find a sequence of DNA which needs to be clipped, and then the Cas 9 will clip that sequence and replace it with the gRNA (Saey TH, 2020). Two ways of applying the CRISPR are-ex vivo (editing outside of body and transport back) and in vivo(send the edited cells into the body) (Figure 2).
Figure 2: The step by step working procedures of CRISPR
Why the CRISPR treatment is so promising is because first, it is faster. CRISPR/Cas9 reduces the time for modification of target genes compared to other technologies that are based on the use of embryonic stem cells (Flora A and Welcker J, 2017). Additionally, a recent study at Johns Hopkins allowed the CRISPR to cut a DNA in response to a specific wavelength of light by engineering a light sensitive RNA molecule; they not only discovered that this engineered CRISPR produced more precise editing, but also that it was faster than traditional methods, cutting about 50% of the targets within 30 seconds (Wasta V, 2020). Some of its accomplishments so far are beneficial to human society. By editing animals or plants’ DNA, the physical traits of these organisms can be modified to remedy long-standing global issues. For example, some types of crops might be prone to pests. Traditional methods of using pesticides can be expensive. In addition heavy reliance on pesticides can lead to gradual higher resistance in pests and contamination of the underground water which pose risks for local communities that rely on this source. Yet, there is a type of corn that has been genetically edited to contain bacteria called Bacillus thuringiensis (BT). It can produce Cry protein, one that can form a hole on the surface of cells that eventually kill those cells, and most importantly, this modification has been proved to be safe for mammals and humans, and its outcome is a 99% decrease in use of pesticide on corns and 95% decrease usage on cottons (Niederhuber M, 2015). Similarly, the CRISPR can also be used for humanistic health aspect, especially when eradicating some diseases that are either acquired or inborn-
“The CRISPR-Cas9 system can be used to manipulate and excise stretches of DNA that have profound relevance for human health, ranging from aggressive malignancies to mitochondrial storage diseases, as well as potential applications in the prevention and treatment of infectious diseases such as human immunodeficiency virus, influenza virus, and malaria, among many others” (McCarthy MW, 2020).
Beyond that, CRISPR can improve people’s lives in both direct and indirect ways. For example, sickle-cell anemia (also known as sickle cell disease or SCD) is a genetic disorder when a patient has a sickle-shaped red blood cell in contrast to the normal disc-shaped red blood cell. DNA has four bases-adenine (A), cytosine (C), guanine (G), and thymine (T). In a person with SCD, a location of A base on his HBB gene was replaced by a T base (Doctrow B, 2021). The mutation sticks hemoglobins together that eventually form the sickle-shaped blood cells. This abnormally shaped cell has a poor ability to transport oxygen in the blood vessels around the body and is more likely to form blood clots. It has the potential to be treated by CRISPR because the patient’s abnormal blood cells can be extracted out of the body and returned back (Issacson W, 2022). The first application of the CRISPR technology on human subjects has successfully taken place on Victoria Gray who has sickle cell anemia. On Stein’s last interview with Gray on December 30, 2021, Gray showed no signs of sickle cell anemia. Additionally, she no longer felt anxious for possible complications and could finish many daily tasks independently (Stein R, 2021). CRISPR also can be used to edit mosquitoes’ genomes, making them infertile, and controlling their population growth; with lower population, the local malaria cases and deaths will decrease objectively. In 2016, around 445,000 people died because of malaria, who are mostly children in Africa, and reducing the mosquito population can significantly reduce the cases and deaths of malaria (Houser K, 2018). Therefore, CRISPR can be used in both human and nonhuman species to improve human health.
Currently, the CRISPR is still undergoing its development, and it will take some time before it can be used widely as a therapeutic means. It will still take a few years for FDA’s approval to become available to the public even if the current result shows the CRISPR technology is safe (Henderson H, 2021). Yet before that, one key problem of CRISPR’s application on allergy therapy needs careful attention-the genetic predisposition factors are the loci on the gene. Editing the whole piece of gene to modify the loci for allergy is both unethical and lethal as it can cause some genetic disorders. We have discovered the direct relation of the HBB gene with the incidence of SCD so that the CRISPR can be applied on SCD patients; yet we haven’t found a gene that leads to the acquisition of allergy. Without further understanding on the pathogenesis of allergy, CRISPR will not be used to treat allergy patients in the short time. Ethical concerns are raised for such a powerful biological tool too. In one case, there are controversies
on how and when CRISPR should be applied on human embryos. While some argued that it is unacceptable to do CRISPR experiment on human embryos after 14 days, it is unlikely for any type of institution to justify what stages a human embryo is now on and whether it has reached its “personhood” (Brokowski C and Adli M 2019). Another ethical concern is on a broader scale. When such tools bring some previously unattainable advantages, would people choose to edit themselves to yield such traits? Issacson W, 2022 includes some definitions for purposes of using the tool like treatment and enhancement. Further, he also coined the idea of “prevention” (editing for avoiding some diseases or disorders) and “super-enhancements” (editing for yielding abilities that never have existed before) in the context of gene-editing. At this point, gene editing creates imbalances, from which the wealthy gain advantages editing the genes of their offspring for favorable traits and eliminating unfavorable ones, leaving the working class incapable of purchasing genetic advantages. Though gene editing for promoting some traits are still fictional, abuse of such a powerful tool would bring disastrous outcomes. In a real world example, He Jiankui, a Chinese scientist at the Southern University of Science and Technology, edited a pair of twins in 2018 in order to prevent HIV from infecting the baby. His finding shocked scientists around the world as the study is deemed highly unethical and questionable. His outcome was a $430,000 fine and being sentenced for 3 years in prison (Johnston J, 2019). Beyond ethical concerns, CRISPR treatment in some cases can be expensive. Taking sickle cell anemia as an example, it is often carried out by somatic editing (modification of cells like bones and blood other than reproductive cells like eggs). However, somatic editing is expensive and might not last for lifetime (Issacson W, 2022); as for sickle cell anemia, its cost can be up to 2 million dollars (Thomas I, 2021). Currently, there are about 100,000 Americans suffering sickle cell anemia (Sickle-cell.com, 2020), but not everyone has 2 million dollars to treat their disease, and unlike common therapies, CRISPR has not yet been covered by insurance. All in all, CRISPR itself is a powerful tool that could potentially solve many current dilemmas faced in many industries, from human healthcare to agriculture; but there are still many existing challenges posed. By overcoming these challenges, CRISPR could be a highly useful and valuable tool that can benefit human society immensely.
Promising solution 2: Sublingual Immunotherapy (SLIT)
Besides genetic treatment, other solutions include mitigating allergy symptoms by exposing the patient to an increasing amount of allergens, which is known as the Allergen Immunotherapy (AIT). This type of treatment is also known as desensitization treatment. This idea was first introduced in the beginning of the 20th century. The first recorded case of using desensitization treatment was done by Leonard Noon in 1911, who treated hay fever by injecting an increasing amount of ragweed into a patient (Luong A, 2009). Afterwards, the allergen immunotherapy developed promptly, and therapies with different functioning regions, or media were developed-one of the first ones was the Subcutaneous Immunotherapy (SCIT), which involves an injection of allergens into tissues under the skin (Figure 3). Other AITs include the Local Bronchial Immunotherapy (LBIT) (the branches in the lung to inhale in oxygen and exhale carbon dioxide), Local Nasal Immunotherapy (LNIT) and Oral Immunotherapy (OIT). However, after a century’s study on them, the LBIT and LNIT was abandoned due to safety reasons. Though the SCIT and OIT left today, they have a higher incidence of side effects after usage. A study in 2018 found about 54.6% immediate and 56.1% delayed local side effects on 581 patients after they received the SCIT injection (Tophof, et al., 2018). Among all the AITs, the sublingual (under tongue) immunotherapy (SLIT) developed last and was accepted by the World Health Organization (WHO in 1998 denoted a potential alternative to SCIT) (Passalacqua G, et al., 2020).
Figure 3: A timeline of the development of sublingual immunotherapy and three of its derivatives that are still accessible till today
The basis for this treatment is simple. It can be done by giving tablets that break down and release a low level of allergen, the threshold for triggering the allergy will be elevated, so the patient will be more tolerant to the allergens. The allergen is placed under the tongue because the dendritic cells, a type of immune cell, are most concentrated in that area. Dendritic cells located in tissues that are exposed to outside environments such as over skins and inner linings of nose, esophagus and stomach (Sidharthan C, 2019). They are powerful antigen presenting cells that connect innate and adaptive immunity and also necessary for the triggering of immune reaction towards external pathogens (Martin-Gayo E and Yu XG, 2019), so the sublingual region would be the most sensitive region in responding to the allergens. Though the mechanism of action of SLIT appears identical to OIT, the later one in fact is also a tablet but works mainly on the dendritic cells that are located in the intestinal lining. Both places have dendritic cells, only the sublingual regions contain more of them. To access the SLIT, a patient will need to have a certificate claiming that he has an allergy, then the medicines will be prescribed under the supervision of a physician. The patient will need to take medicine drops under his tongue daily, and the whole treatment can last years or more. With increasing doses of allergens, the patient’s sensitivity to the allergens decreases over time. Even without taking medication for several years after the treatment, his or her body will retain a high tolerance for these allergens. The SLIT treatment does sound miraculous and has been proven to be effective. A 2014 study showed a “clinical meaningful” reduction in ragweed allergies in a Canadian population, dependent on seasons and mild to subtle complications (Kim H, et al., 2014). Other studies include a meta-analysis done in 2006 analyzed data on 484 patients aged 3 to 18 with allergic rhinitis in which they found that after immunotherapy there was an obvious reduction in symptom incidence and medication use (Penagos M, et al., 2006). In addition, it has more advantages over some conventional treatments. This stands for two features-the sublingual therapy’s convenience and safety. Traditional therapies are composed mainly of injections; for example, the subcutaneous injection needs a patient 1-2 allergy shots per week for 6 consecutive months, then receive maximum dose once every 2-4 weeks (Reshamwala N, 2021). On the other hand, sublingual therapy does not require patients to go to clinics for each treatment, neglecting trips to the clinics, a patient can take tablets anywhere. The therapy has also been proved to be safe years after its approval. Although the occurrence of anaphylaxis and its symptoms is not eliminated, a study estimated 2.7 cases of allergic reactions among 1,000 SLIT doses, with 0.056% of severe reactions that are safer than SCIT (James C and Bernstein DI, 2017). The sublingual immunotherapy is so popular that about 45% European patients have access to it; according to a survey done in 2018 on 268 US allergists, 197 of them announced that they prescribe allergy tablets (Heights A, 2021). Price is also a factor in evaluating the availability of the treatment. Fortunately compared to other treatments, the sublingual immunotherapy is more affordable. The price is not covered by insurance ranges from $500-$2100 depending on antigen treatments and practices applied (Seiberling K, et al., 2012). Considering the effectiveness, convenience and affordability, sublingual immunotherapy is likely to be one of the most popular solutions for patients with allergy and anaphylaxis contemporarily.
The SLIT does have some flaws people should review before they decided to take it. First, patients have limited options for SLIT treatment. Not only because the sublingual drops have not been approved by the FDA yet, the current FDA-approved SLIT tablets are only for patients who are allergic to certain allergens like pollen, dusts and some grasses. Currently there are four brands of tablets approved by FDA for usage-
• Odactra (for people aged 18-65 with dust mite allergy)
• Grastek (for people with timothy grass allergy)
• Oralair (for people aged 10-65 with allergic rhinitis)
• Ragwitek (for people with ragweed allergy) (American Academy of Allergy Asthma and Immunology, 2020).
Although sublingual tablets aimed for patients with food allergies to kiwi, peanut and milk are improving and making progress in recent years, such treatments haven’t been approved by the FDA yet (FDA, 2022; KSAT, 2015). As such, they are usually inaccessible to the public as these tablets are held by a few selected allergists. Second, noticing that the tablets fight against allergy by building up tolerance, this process can take a long time. Although the definite course of treatment is still unclear, duration of at least 3 years could provide lasting benefits after the discontinuation (Creticos PS, 2022). In addition, during these years, the efficacy of tablets depends highly on the patient’s adherence toward the treatment, meaning the effect relies on whether the patient continues taking tablets daily. A study in 2010 analysed the percentage of adherence from marketing data in two Italian tablet manufactures and what they found is less optimistic than the survey. 50% after the first year and about 15% persisted three years of treatment across all regions, contrary to 95% reported in the survey (Senna G, et al., 2010). In all long-term therapies, patients’ adherence is one of the top factors in determining the efficacy of the treatment, and this study did not find a plausible and general reason to conclude all the discontinuation cases. Although sublingual immunotherapy poses several challenges, the benefits outweigh the disadvantages, as the flaws are relatively more avoidable compared to other solutions. Therefore, it is clear that sublingual immunotherapy has the potential to become one of the most powerful and effective treatments for anaphylactic allergies.
Promising solution 3: Biological and antibody medications
For the two solutions mentioned above, they can either lower the occurrence of allergy, reduce the incidence of severe allergic reactions, or mitigate the severity of allergic symptoms. Over many decades of development, other common treatments (medicines) are in plentiful forms including tablets, spray, and eye drops. Depending on a varied treatment mechanisms and subsequent routes of administration, they have different effects on different groups of people. In considering medication for allergies, many factors are scrutinized such as safety, efficacy, affordability, and dose. Here are some mechanisms that show how various types of medications work.
Mechanism type one-antihistamine: Histamine is stored inside of mast cells (a type of immune cell that can trigger allergic response) around the body and is released by contact with immunoglobulin secreted from the B cells. It has many psychological jobs, including cell differentiation, proliferation, haematopoiesis (production of red blood cell), and cell regeneration (Branco AC, et al., 2018); nonetheless, its primary function is to trigger inflammatory responses, and in allergy patients’ cases, histamines are produced excessively. Once histamines are released, they bind to the histamine receptors on the surface of cells (H1, H2, H3 and H4 receptors), in which binding to the H1 receptor is usually the cause of allergy (Robertson S, 2019). Therefore one of the solutions to the allergy is to reduce histamine binding with the receptor, which is the antihistamine drugs (specifically H1 receptor antagonist) work. Currently the accessible antihistamine medications can be categorized to two groups-first generation (FDA approved after 1930s) and second generation (FDA approved after 1980s). The second generation is deemed as more preferable for it does not cross the brain-blood barrier that can cause drowsiness as the first generation do (Cleveland Clinic, 2020). This is a significant improvement, because this sedative effect can be detrimental in cases of addiction. FDA has announced that overdosing of Benadryl (a type of first generation antihistamine) can cause cardiac problems, coma and even death (FDA, 2020). Meanwhile, antihistamine is affordable and some of which are covered by health insurance.
Mechanism type two-decongestant: When we have cold or allergic reactions, we generally will develop a runny nose. The mechanism of inducing a runny nose varies, while for patients with allergic rhinitis, they will most likely develop nasal inflammation; in which eventually lead to the expansion of the nasal venous sinusoid, swelling of nasal turbinates (a bony structure inside of nose that make the incoming air warm and moist) and block the airflow in nostrils, and cause nasal Decongestant is another type of medication that aims to help patients who are mainly suffering from a runny nose that is caused by cold or allergic rhinitis. Currently there are several ways of delivering-nasal spray, tablets and eye drops, and there are two separate mechanisms of decongestants-topical and systemic. Topical decongestant works on a specific organ while systemic works by the circulation on the whole body.
The way decongestant works is by binding to the alpha-adrenergic receptor to reduce the release of certain neurotransmitters, and thereby to stimulate the vasodilation (relaxation). There are two main types of alpha receptors-alpha-1 (a1) and alpha-2 (a2). The alpha-1 receptor works on mainly determining the blood pressure, and the alpha-2 receptor works on determining the sympathetic outflow (one that can increase physical arousal) and might be able to control regional blood flow (Reid JL, 1986). By direct binding to such receptors found in the nasal mucosa with their sympathomimetic agents, vasoconstriction (the process where blood vessels become narrower) will happen and mitigate the swelling of local tissues (Johnson DA and Hricik JG, 1993). Common decongestants that are available are primarily alpha-1 based agonists (a substance that triggers physiological response when binding to its receptor), but those that work on alpha-2 receptors are developing too. A study tested the efficacy of alpha-2 agonist BHT-920 and PGE-6201204 on dogs, pigs and monkeys in 2007 showed the relevance of alpha-2 based agonist and vasoconstrictor effect, which can elicit decongestion response (Corboz MR, et al., 2007). The difference between decongestants with different based alpha-adrenergic receptors on their safety. The same team observed the decongestant effect of BHT-920 on a pig nasal explant and an in vivocat model of congestion in the next year. They found out that those alpha-2 based agonists provide a normal decongestant effect, while also preventing side effects like high blood pressure that other decongestants may have (Corboz MR, et al., 2007). The problem with the decongestant is that there has not been a consensus about the efficacy of decongestant. The meta-analysis done in 2016 on 15 studies found that the efficacy is largely affected by patients’ subjective feedback, and six of the studies were funded by unclear sources (Meth M, 2022). Despite these concerns, for those who may have allergic rhinitis or nasal congestion, decongestant is one ideal solution for them.
Mechanism type three-mast cell stabilizer: Mast cell stabilizer is another option for patients with allergy. As its name implies, its target is solely the mast cell, a type of immune system cell located in connective tissue all around the body. It is best known for having many receptors and granules of proteins. When it is exposed to pathogens, its receptor binds to the IgE from the type B cell and the mast cell releases all of its granules. The release of inflammatory mediators is known as degranulation and includes the release of histamine when mast cells encounter allergens. The chemicals released could cause inflammation of the local area, dilate the vessels and slow the blood movement, so that antibodies and other immune system cells might travel along the blood vessels, coming to the injured area and fight the pathogens. After all the pathogens have been eliminated, the Corticotropin Releasing Factor subtype 2 (CRF 2) will signal to stop the degranulation (Lenhard E, 2022). In allergy cases, the CRF 2 might be insufficient to stop the degranulation on time, causing a prolonged period of inflammation, therefore the mast cell stabilizer works like CRF 2 to inhibit further degranulation process. For now there are many brands of mast cell stabilizer, and they have a slightly different mechanism of action from each other; for example, lodoxamide (Alomide), a type of mast cell stabilizer that focus on eye inflammations, works by increasing the vascular permeability, which limit IgE and antibodies’ ability to pass across the blood vessels to tissues (PubChem, 2022). While most others, like Cromolyn sodium (a calcium channel inhibitor), can restrain the release of mediators that can induce inflammation directly. How such types of medicines work is by blocking the calcium channels on the mast cells so that they are prevented from receiving signals of performing further degranulation (Chand N, et al., 1986). The disadvantage of the mast cell stabilizer class is its pharmacology. Oka T, et al., 2012 performed a study to discover the efficiency of Cromolyn in reducing the bodily response. Their studies were done on mice, and they have confirmed that Cromolyn functioned to reduce the mast cell’s activation, but it did not alleviate the existing ear swelling symptoms of mice. The result indicates that mast cell stabilizer (at least the Cromolyn) is not like normal medicines that can relieve symptoms in certain areas, but rather provides a preventative effect on people. Apart from that, it has some advantages. Although bearing some side effects, there have been no reports of serious outcomes decades after its introduction, and brands in eye drop media cost no more than $300 (Cardin D, 2022).
Mechanism type four-steroids (Corticosteroids): Though more commonly known as performance enhancers, steroids can also be used to treat inflammation symptoms. This is due to two classes of steroids. One that is prohibited by sports competition is called anabolic steroid, while the one used to treat inflammation is called corticosteroid. Steroid is an artificial version of hormone usually produced by the adrenal glands above the kidneys. It can reduce the redness and swelling, and also inhibit the immune system activity; therefore it has an immunosuppressive effect (NHS, 2020; NHS, 2021). Meanwhile further classification of corticosteroid includes glucocorticoids and mineralocorticoids. Their difference stands at their function while glucocorticoids help activate the immune cells, mineralocorticoids work on the regulation of blood volume and pressure (Taves MD, et al., 2011). In this case it is glucocorticoids that are used for allergy treatment (Lindner B, 2019). It helps to alleviate allergic reactions by either binding to the glucocorticoids receptors directly, or interacting with transcription factors especially protein-1 and nuclear factor-kappaB (van der Velden VH, 1998). One criteria of taking the corticosteroid that needs careful consideration is its safety from dosage. As overuse may result in osteoporosis (bones becoming fragile), avascular necrosis (malfunctioning of bones due to little or no blood supply), glaucoma (gradual loss of sight) and diabetes (lack of insulin in bloodstream) (Youssef J, et al., 2016). Fortunately, corticosteroids are one of the most economical options. Prednisone, one of the most common types of corticosteroid, costs no more than $10 for most patients.
Conclusion
Until now, there have been few, if any, ways of eradicating allergies completely. Compared to the solutions presented, desensitization therapy, especially sublingual immunotherapy, stands out as the most promising solution as it has already been proven as a safe option in European countries. Yet it prevents people from severe allergic responses, not removing one from any contact with allergens. One of its biggest obstacles is getting approval from the American Food and Drug Administration (FDA). Standards like the drugs’ safety, efficacy, whether its potential benefits outweigh the risks and whether its manufacturer meets the federal quality standards are being evaluated. In SLIT’s case, the studies were done under slightly different settings, (conditions like allergen exposure and extent to which patients have symptoms of), making it hard to reach a conclusion of whether the drug should be approved. Its future is still unknown, but developments of SLIT tablets on food allergies are ongoing. Gene editing technology is still a promising solution, yet more understanding on human genetics and allergic inheritance and relevant policies need to be achieved before gene editing can be utilized as a treatment for anaphylaxis.
As for medicines and drugs, the main point is to find one that is suitable for individuals. Though most brands in three (antihistamine, decongestant, corticosteroid) out of four medicines listed are available as over-thecounter medications, it is better for those who never used such drugs before to ask pharmacists or private health-care providers. With different individual body situations and allergies, their options can be different. In some cases, the patient might need to avoid certain classes of medications for their body is sensitive to a type of drug ingredient; in rare cases, their body could be allergic to certain ingredients that one or many brands of medicines may contain. An interview in 2015 showed a woman named Sandy who was later found to be hypersensitive to both seasonal allergies and chemicals in certain allergy medicines. Choosing those approved from FDA and seeking advice from relevant experts is important things to contemplate in advance.
Acknowledgement
I would like to thank my mentor Ms.Collins for her guidance throughout the writing of this article. Without her patience and detailed comment this work would not have been possible.
References
- Hirsch L. Kids and allergies. Nemours kidsHealth. 2022.
- Rubinstein R. How allergies interfere with your life. Hodson Valley Sinus Center. 2018.
- Jaruvongvanich V, Mongkolpathumrat P, Chantaphakul H, Klaewsongkram J. Extranasal symptoms of allergic rhinitis are difï¬cult to treat and affect quality of life. Allergol Int. 2016; 65(2): 199-203.
[Crossref] [Google scholar] [Pubmed]
- Heggie J. A brief history of allergies. National Geographic. 2018.
- Shampo MA, Kyle RA. Daniel Bovet-nobel laureate in medicine. Mayo Clin Proc. 1999; 74(10): 1016.
[Crossref] [Google scholar] [Pubmed]
- The first 5,000 years of allergy care. Charlotte Eye Ear Nose and Throat Associates. 2018.
- Benedek TG. History of the development of corticosteroid therapy. Clin Exp Rheumatol. 2011; 29(5 Suppl 68): 5-12.
[Google scholar] [Pubmed]
- Allergy facts. ACAAI Public Website. 2021.
- Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006; 368(9537): 733-743.
[Crossref] [Google scholar] [Pubmed]
- What are Genome Wide Association Studies (GWAS)? GWAS Catalog. 2023.
- Uffelmann E, Huang QQ, Munung NS, de Vries J, Okada Y, Martin AR, et al. Genome-wide association studies. Nat Rev Methods Primers. 2021; 1(1): 59.
- Brookshire B. Scientists say: Loci. ScienceNewsExplores. 2019.
- Bønnelykke K, Sparks R, Waage J, Milner JD. Genetics of allergy and allergic sensitization: Common variants, rare mutations. Curr Opin Immunol. 2015; 36: 115-26.
[Crossref] [Google scholar] [Pubmed]
- Indoor air pollution: The invisible enemy of allergy sufferers. Sanofi. 2019.
- Jenerowicz D, Silny W, Danczak-Pazdrowska A, Polanska A, Osmola-Mankowska A, Olek-Hrab K. Environmental factors and allergic diseases. Ann Agric Environ Med. 2012; 19(3).
[Google scholar] [Pubmed]
- Igea JM. The history of the idea of allergy. Allergy. 2013; 68(8): 966-973.
[Crossref] [Google scholar] [Pubmed]
- Gotter A. Anaphylactic shock: What you need to know. Healthline. 2019.
- Lieberman P, Camargo Jr CA, Bohlke K, Jick H, Miller RL, Sheikh A, et al. Epidemiology of anaphylaxis: Findings of the American college of allergy, asthma and immunology epidemiology of anaphylaxis working group. Ann Allergy Asthma Immunol. 2006; 97(5): 596-602.
[Crossref] [Google scholar] [Pubmed]
- Borish L, Danoff T, Ma LL. Death from anaphylaxis is a reassuringly unusual outcome. J Allergy Clin Immunol. 2014; 133(2): AB234.
- John P. Allergic cascade: Get facts on the symptoms and treatment. MedicineNet. 2021.
- Biology for majors II: Antigen presenting cells. Lumen. 2020.
- Restak R. Protection in the body: A complete user's guide. 2014.
- Bowden ME. A mighty pen. Science History Institute. 2021.
- Kaplan S. EpiPen® Auto-injector: U.S. patent No. 4,031,893. 2016.
- Hormonal control of osmoregulatory functions-epinephrine and norepinephrine. LibreTexts Biology. 2022.
- Sharma H. How does epinephrine turn off an allergic reaction? Allergic Living. 2020.
- Tunney K. How many people use Epipens in America? Mylan’s price increase is taking advantage of its users. Bustle. 2016.
- Elenburg S, Blaiss MS. Current status of sublingual immunotherapy in the United States. World Allergy Organ J. 2014; 7(1): 1-7.
[Crossref] [Google scholar] [Pubmed]
- Rubin R. EpiPen price hike comes under scrutiny. Lancet. 2016; 388(10051): 1266.
[Crossref] [Google scholar] [Pubmed]
- Marsh T. Generic Epipen is still expensive-here's how you can save. GoodRx Health. 2019.
- Morris SY. Everything you should know about biphasic anaphylaxis. Healthline. 2020.
- Hamilton DK. Is emergency room care after home use of an epinephrine auto injector always needed? J Allergy Clin Immunol. 2019; 143(2): AB265.
- Lander ES. The heroes of CRISPR. Cell. 2016; 164(1-2): 18-28.
[Crossref] [Google scholar] [Pubmed]
- Saey TH. Explainer: How CRISPR works. ScienceNewsExplores. 2020.
- Flora A, Welcker J. CRISPR genome engineering: Advantages and limitations. Taconic Biosciences. 2017.
- Wasta V. Light-activated 'CRISPR' triggers precision gene editing and super-fast DNA repair. Johns Hopkins Medicine Newsroom. 2020.
- Niederhuber M. Insecticidal plants: The tech and safety of GM Bt crops. Science in the News. 2015.
- McCarthy MW. Harnessing the potential of CRISPR-based platforms to advance the field of hospital medicine. Expert Rev Anti Infect Ther. 2020; 18(8): 799-805.
[Crossref] [Google scholar] [Pubmed]
- Doctrow B. Fixing the sickle cell disease gene. National Institutes of Health (NIH). 2021.
- Isaacson W. The code breaker-young readers edition: Jennifer Doudna and the race to understand our genetic code. 2022.
- Stein R. First sickle cell patient treated with CRISPR gene-editing still thriving. NPR. 2021.
- Houser K. Genetically engineered mosquitoes are about to fly free in Africa. Neoscope. 2018.
- Henderson H. CRISPR clinical trials: A 2019 update. Innovative Genomics Institute. 2021. [Crossref]
- Brokowski C, Adli M. CRISPR ethics: Moral considerations for applications of a powerful tool. J Mol Biol. 2019; 431(1): 88-101.
[Crossref] [Google scholar] [Pubmed]
- Johnston J. He jiankui is going to jail. Would the U.S. criminally prosecute a rogue gene-editing researcher? STAT. 2019.
- Thomas I. How CRISPR gene editing will treat diseases in future: Nobel-winning Intellia co-founder Jennifer Doudna. CNBC. 2021
- How common is sickle cell disease? Sickle-cell.com. 2020.
- Luong A. Understanding the mechanism of allergen immunotherapy. UTHealth Houston-McGovern Medical School. 2009.
- Tophof MA, Hermanns A, Adelt T, Eberle P, Gronke C, Friedrichs F, et al. Side effects during subcutaneous immunotherapy in children with allergic diseases. Pediatr Allergy Immunol. 2018; 29(3): 267-274.
[Crossref] [Google scholar] [Pubmed]
- Passalacqua G, Bagnasco D, Canonica GW. 30 years of sublingual immunotherapy. Allergy. 2020; 75(5): 1107-1120.
[Crossref] [Google scholar] [Pubmed]
- Sidharthan C. What are dendritic cells? News Medical Lifesciences. 2019.
- Martin-Gayo E, Yu XG. Role of dendritic cells in natural immune control of HIV-1 infection. Front Immunol. 2019; 10: 1306.
[Crossref] [Google scholar] [Pubmed]
- Kim H, Waserman S, Hébert J, Blaiss M, Nelson H, Creticos P, et al. Efficacy and safety of ragweed sublingual immunotherapy in Canadian patients with allergic rhinoconjunctivitis. Allergy Asthma Clin Immunol. 2014; 10(1): 1-9.
[Crossref] [Google scholar] [Pubmed]
- Penagos M, Compalati E, Tarantini F, Baena-Cagnani R, Huerta J, Passalacqua G, et al. Efficacy of sublingual immunotherapy in the treatment of allergic rhinitis in pediatric patients 3 to 18 years of age: A meta-analysis of randomized, placebo-controlled, double-blind trials. Ann Allergy Asthma Immunol. 2006; 97(2): 141-148.
[Crossref] [Google scholar] [Pubmed]
- Reshamwala N. Traditional immunotherapy in Austin. Frontier Allergy Asthma & Immunology. 2021.
- James C, Bernstein DI. Allergen immunotherapy: An updated review of safety. Curr Opin Allergy Clin Immunol. 2017; 17(1): 55.
[Crossref] [Google scholar] [Pubmed]
- Heights A. New research shows 73 percent of allergists prescribe under-the-tongue allergy tablets. ACAAI Public Website. 2019.
- Seiberling K, Hiebert J, Nyirady J, Lin S, Chang D. Cost of allergy immunotherapy: Sublingual vs. subcutaneous administration. Int Forum Allergy Rhinol 2012; 2(6): 460-464.
[Crossref] [Google scholar] [Pubmed]
- Sublingual immunotherapy (slit) allergy tablets. American Academy of Allergy Asthma and Immunology. 2020.
- Is it really 'FDA approved'? US Food and Drug Administration (FDA). 2022.
- Allergic to allergy medicine! KSAT. 2015.
- Creticos PS. Sublingual immunotherapy for allergic rhinitis and conjunctivitis: SLIT-tablets. UpToDate. 2022.
- Senna G, Lombardi C, Canonica GW, Passalacqua G. How adherent to sublingual immunotherapy prescriptions are patients? The manufacturers' viewpoint. J Allergy Clin Immunol. 2010; 126(3): 668-669.
[Crossref] [Google scholar] [Pubmed]
- Branco AC, Yoshikawa FS, Pietrobon AJ, Sato MN. Role of histamine in modulating the immune response and inflammation. Mediators Inflamm. 2018.
[Crossref] [Google scholar] [Pubmed]
- Robertson S. Histamine mechanism. News. 2019.
- Antihistamines. Cleveland Clinic. 2020.
- FDA warns about serious problems with high doses of the allergy medicine diphenhydramine (Benadryl). US Food and Drug Administration (FDA). 2020.
- Naclerio RM, Bachert C, Baraniuk JN. Pathophysiology of nasal congestion. Int J Gen Med. 2010: 47-57.
[Crossref] [Google scholar] [Pubmed]
- Reid JL. Alpha-adrenergic receptors and blood pressure control. Am J Cardiol. 1986; 57(9): E6-E12.
[Crossref] [Google scholar] [Pubmed]
- Johnson DA, Hricik JG. The pharmacology of αâ?adrenergic decongestants. Pharmacotherapy. 1993; 13(6P2): 110S-115S.
[Crossref] [Google scholar] [Pubmed]
- Corboz MR, Mutter JC, Rivelli MA, Mingo GG, McLeod RL, Varty L, et al. α2-adrenoceptor agonists as nasal decongestants. Pulm Pharmacol Ther. 2007; 20(2): 149-156.
[Crossref] [Google scholar] [Pubmed]
- Meth M. The best nasal decongestants by age. Medical News Today. 2022.
- Lenhard E. Don't overreact: Research pinpoints mast cell receptor in immune response, disease signs. Michigan State University-The College of Veterinary Medicine. 2022.
- Lodoxamide. PubChem. 2022.
- Chand N, Perhach JL, Diamantis W, Sofia RD. Heterogeneity of calcium channels in mast cells and basophils and the possible relevance to pathophysiology of lung diseases: A review. Agents Actions. 1986; 17: 407-417.
[Crossref] [Google scholar] [Pubmed]
- Oka T, Kalesnikoff J, Starkl P, Tsai M, Galli SJ. Evidence questioning cromolyn’s effectiveness and selectivity as a ‘mast cell stabilizer’in mice. Lab Invest. 2012; 92(10): 1472-1482.
[Crossref] [Google scholar] [Pubmed]
- Cardin D. Mast cell stabilizers: Uses, common brands, and safety info. SingleCare. 2022.
- Steroids. National Health Service (NHS). 2020.
- Allergies. NHS inform. 2021.
- Taves MD, Gomez-Sanchez CE, Soma KK. Extra-adrenal glucocorticoids and mineralocorticoids: Evidence for local synthesis, regulation, and function. Am J Physiol Endocrinol Metab. 2011; 301(1): E11-E24.
[Crossref] [Google scholar] [Pubmed]
- Lindner B. How do allergy drops work over the course of allergy treatment? Allergy Associates of La Crosse. 2019.
- van der Velden VH. Glucocorticoids: Mechanisms of action and anti-inflammatory potential in asthma. Mediators Inflamm. 1998; 7(4): 229-237.
[Crossref] [Google scholar] [Pubmed]
- Youssef J, Novosad SA, Winthrop KL. Infection risk and safety of corticosteroid use. Rheum Dis Clin North Am. 2016; 42(1): 157-176.
[Crossref] [Google scholar] [Pubmed]
Author Info
Zhihan Cui*Citation: Cui Z: Potential Treatments for Allergies and Anaphylaxis
Received: 20-Mar-2023 Accepted: 04-Apr-2023 Published: 11-Apr-2023, DOI: 10.31858/0975-8453.14.4.248-255
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3