Case Report - (2023) Volume 14, Issue 3
Abstract
This study is about an infrequent first presentation of Aortic Dissection (AD), and it is primary Ventricular Fibrillation (VF). We present a 64-year-old woman with a history of hypertension who came with sudden retrosternal chest pain, dizziness, nausea, and vomiting. The patient suffered a cardiac arrest a few seconds after admission. Cardiopulmonary Resuscitation (CPR) was done for her. An Electrocardiogram (ECG) showed ST elevation that demonstrated acute anterior MI (Myocardial Infarction). Trans-thoracic echocardiography (echo), Computed Tomography Angiography (CTA) demonstrated decreased Left Ventricular Ejection Fraction (LVEF) with standard LV size (LVEF=25%) and type A Stanford and type I DeBakey Aortic Dissection flap from root up to distal of abdominal Aorta. This is while the patient’s first presentation was VF, and she had anterior MI, which is unusual for Aortic Dissection. Therefore, we must consider AD in patients with VF. We have to consider AD in anterior MI patients because of the contraindication of medication.
Keywords
Aortic Dissection (AD), Ventricular Fibrillation (VF), Anterior Myocardial Infarction (MI), Electrocardiogram (ECG)
Introduction
Aortic Dissection (AD) is a rare, life-threatening condition that occurs when the damaged internal layer of the aorta results in blood flowing throw the layers of the aorta. We cannot use antiplatelet and anticoagulant drugs because of the surgery situation in type A AD, but we have to use antiplatelet and anticoagulant drugs in Acute Myocardial Infarction (AMI) (Núñez-Gil IJ, et al., 2015). In this case, Ventricular Fibrillation (VF) and ST-segment elevation guide us to AMI and the use of antiplatelet and anticoagulant drugs and interventional procedures like catheterization. However, they should not be used in type A Stanford AD. Therefore there is a difficult situation in type A AD patients, even in differential diagnosis and follow-up.
Case Presentation
A 64-year-old woman with a history of hypertension was admitted to the emergency department of Imam Hossein Hospital in Shahroud at 9:00 am with sudden retrosternal chest pain (burning and spreading to the arms), dizziness, nausea, and vomiting. Blood pressure (103/63 mm Hg), pulse rate (78 b/min), respiration rate (14 BPM), oxygen saturation (96%), blood sugar (180), and temperature (36ºC) were checked. Cardiac auscultation sounds were clear, and S1 and S2 in cardiac auscultation were heard. Pulmonary auscultation was clear. She has no history of food or drug allergies and does not take any specific medications, and has no other medical condition. She did not use any medicine for her hypertension and had uncontrolled hypertension.
The first ECG was taken at 9:15 am, and it showed recurrent Premature Ventricular Contractions (PVC) (Figure 1A). She suffered a cardiac arrest a few seconds after the first ECG. Cardiopulmonary Resuscitation (CPR) was done for her, and she received two shocks. The following ECG after successful CPR showed ST elevation in pericardial leads (V2-V6), and we found out that the arrest occurred in the field of acute anterior MI (Figures 1B and 1C). A 7.5 endotracheal tube was inserted, and she was connected to a ventilator. After 10 minutes of CPR, the rhythm became almost normal.
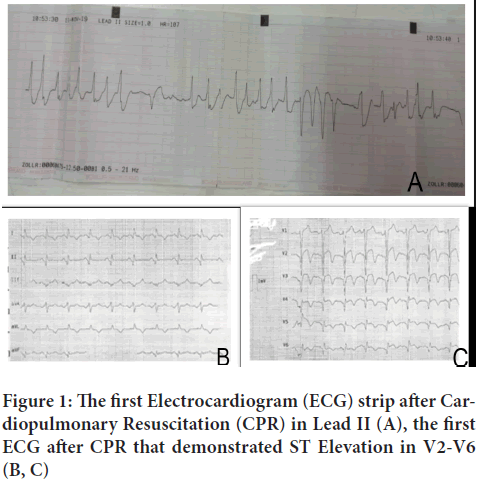
Figure 1: The first Electrocardiogram (ECG) strip after Cardiopulmonary Resuscitation (CPR) in Lead II (A), the first ECG after CPR that demonstrated ST Elevation in V2-V6 (B, C)
Pantazole 40 mg IV and Ondansetron 4 mg IV were prescribed. A cardiologist visited the patient, and a paraclinical examination was done (Table 1).
| Components | Test results | Normal range |
|---|---|---|
| WBC (White Blood Cells) | 13000 | 4.5-11.0 × 109/L |
| RBC (Red Blood Cells) | 3.85 | 4.2-5.4 million cells/mcL |
| BS (Blood Sugar) | 163 | <140 mg/dL |
| MCV (Mean Cell Volume) | 91.1 | 80-100 fL |
| MCH (Mean Corpuscular Hemoglobin) | 30.1 | 27.5-33.2 Picograms |
| Troponin | Negative | |
Table 1: Hematology and biochemistry tests
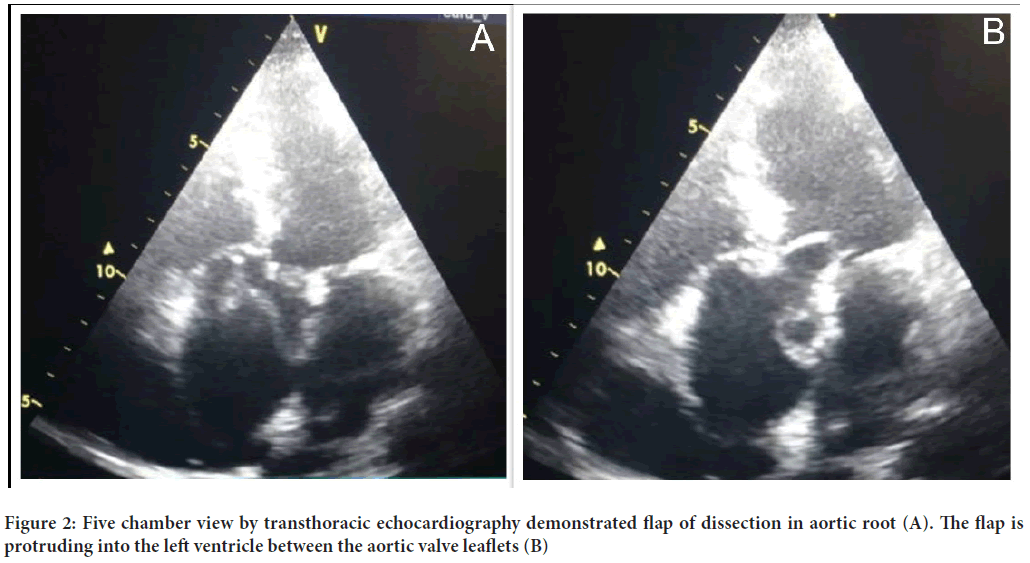
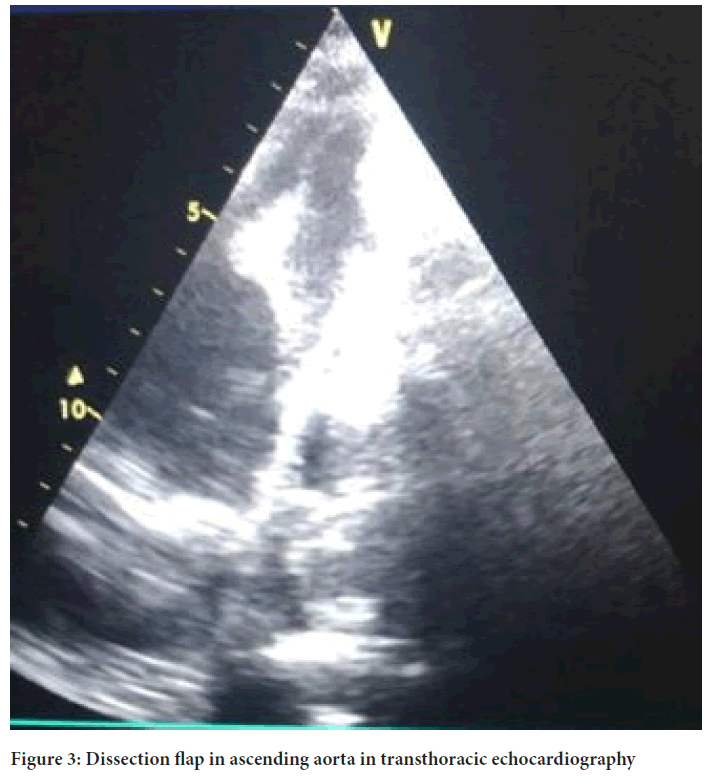
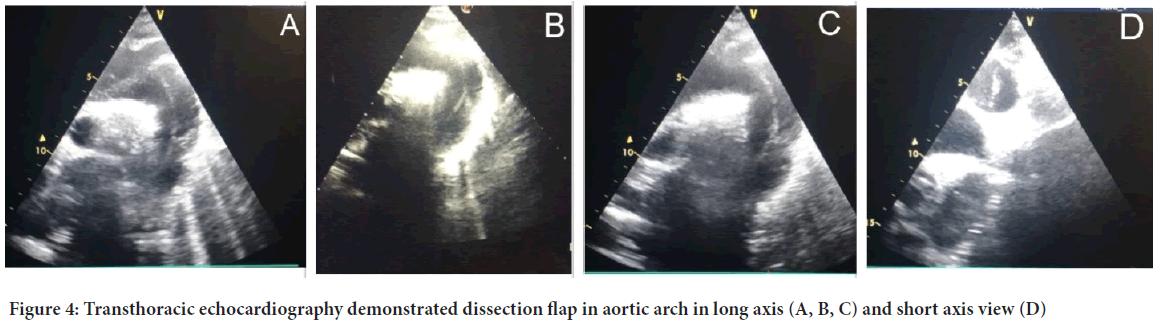
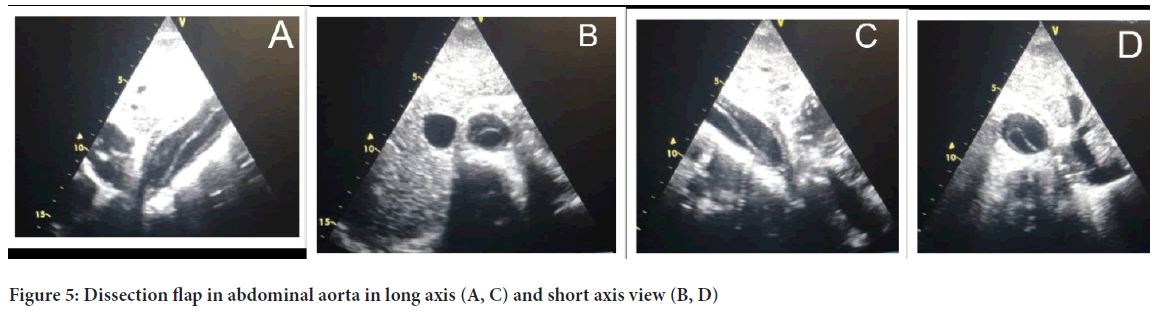
Trans-thoracic echocardiography was done in the emergency room that demonstrated decreased Left Ventricular Ejection Fraction with normal LV size (LVEF=25%) and Aortic Dissection flap from root up to distal of abdominal Aorta (Figures 2-5). CT angiography of the Aorta and coronary arteries demonstrated patient epicardial coronary arteries and was in favor of Aortic Dissection type A Stanford and type I DeBakey (Figure 6). This method is used while the patient had an anterior MI.
Figure 2: Five chamber view by transthoracic echocardiography demonstrated flap of dissection in aortic root (A). The flap is protruding into the left ventricle between the aortic valve leaflets (B)
Figure 3: Dissection flap in ascending aorta in transthoracic echocardiography
Figure 4: Transthoracic echocardiography demonstrated dissection flap in aortic arch in long axis (A, B, C) and short axis view (D)
Figure 5: Dissection flap in abdominal aorta in long axis (A, C) and short axis view (B, D)
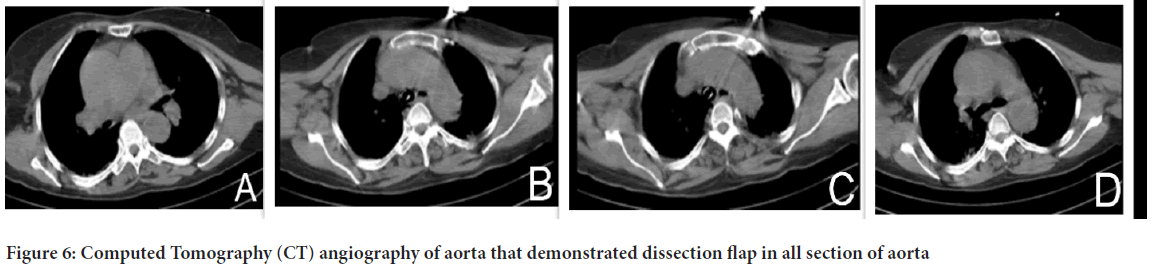
Figure 6: Computed Tomography (CT) angiography of aorta that demonstrated dissection flap in all section of aorta
The patient’s vital signs were controlled every five minutes, and the last one was done at 6:45 pm blood pressure (114.53 mm Hg), pulse (59 b/min), respiratory rate (12 BPM), oxygen saturation (100%), temperature (37°C). The patient needed surgery as soon as possible, and since our hospital did not have the necessary facilities for cardiovascular surgery, she was transferred to a center with these facilities.
Results and Discussion
AD symptoms may be similar to those of other heart disorders; AD is frequently confused with myocardial ischemia leading to a delayed or misdiagnosis, resulting in inappropriate treatment, including the use of antithrombotic agents (Harris KM, et al., 2010).
When a dissection flap extends proximally, it may impinge on the orifice of one of the coronary arteries resulting in Acute Myocardial Infarction (AMI) or ischemia. The dissection channel frequently propagates along the greater curvature of the aorta and may compromise the Ostia of the arch vessels. Given its location on the greater curvature, the right coronary artery is particularly vulnerable to occlusion, which helps explain why most Myocardial Infarctions complicating Aortic Dissection are inferior in location. However, for patients with AMI, the missed diagnosis of AD could be catastrophic because antiplatelet therapy and cardiac catheterization, which are the therapeutic approaches for AMI, are exactly two absolute contraindications to AD treatment, as both of them can aggravate bleeding, broaden the range of the dissection, and even increase the risk of death (Hagan PG, et al., 2000; Windecker S, et al., 2014).
In approximately 17% of cases, pain can change location and follow the dissection path. Moreover, some patients shows other signs like loss of consciousness, shortness of breath, sudden difficulty speaking, loss of vision, weakness or paralysis of one side of the body, similar to those of a stroke, and weak pulse in one arm or thigh compared with the other arm, leg pain, difficulty walking, leg paralysis, nausea, and vomiting (JCS Joint Working Group, 2013).
Standard tests used to diagnose aortic incision include a chest iodine CT scan and an echocardiogram (sensitivity of 77% to 80% and a specificity of 93% to 96%(. Transthoracic Echocardiography (TTE) and Transesophageal Echocardiography (TEE) can be performed quickly for hemodynamically unstable patients. The TEE can identify the entry site of dissection, the presence of false lumen thrombus, the presence of an undulating intimal flap that differentiates the false lumen from the true lumen, the involvement of arch and coronary vessels, pericardial effusion, and the severity of aortic valve regurgitation. Other tests that may be used include an aortogram or angiogram of the aortic magnetic resonance or a higher frequency ultrasound. Measurement of blood D-dimer level may be helpful in diagnostic evaluation. Each of these tests has pros and cons and does not have the same sensitivity and characteristics in diagnosing Aortic Dissection (Nienaber CA and Clough RE, 2015).
10% of type B dissection patients have electrocardiographic signs of ischemia. So, differential diagnosis should be performed on all patients to differentiate pain from AMI and AD. A normal ECG was seen in one-third of patients, and ECG showed non-specific ST-and T-wave changes in 42%, ischemic changes in 15%, and evidence of Acute Myocardial Infarction in 5% of patients with an ascending Aortic Dissection (Bossone E, et al., 2013).
The chest X-ray is not sufficient to rule out or diagnose Aortic Dissection; however, it has been reported abnormal in 60%-90% of patients (Siegal EM, 2006).
AD and AMI may have onset with acute chest pain, and it is sometimes difficult to diagnose them by symptoms, ECG changes, and/or cardiac biomarkers.
Conclusion
Our case was presented with ECG changes in ST elevation and VF, which was similar to anterior MI. The physician did echocardiography to confirm his diagnosis and noticed Aortic Dissection, according to the witness, while for Aortic Dissection we expect inferior MI to occur. This study states that we have to consider Aortic Dissection in patients with the presentation of arrhythmia, especially Ventricular Fibrillation (VF), even if Myocardial Infarction has been demonstrated in them.
Declarations
Ethical approval
Research committee of Shahroud University of Medical Sciences has approved this study.
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Availability of data and materials
The datasets used during the current study are available from the corresponding author upon reasonable request.
References
- Núñez-Gil IJ, Bautista D, Cerrato E, Salinas P, Varbella F, Omedè P, et al. Incidence, management, and immediate and long-term outcomes after iatrogenic aortic dissection during diagnostic or interventional coronary procedures. Circulation. 2015; 131(24): 2114-2119.
[Crossref] [Google Scholar] [Pubmed]
- Harris KM, Strauss CE, Duval S, Unger BT, Kroshus TJ, Inampudi S, et al. Multidisciplinary standardized care for acute aortic dissection: Design and initial outcomes of a regional care model. Circ Cardiovasc Qual Outcomes. 2010; 3(4): 424-430.
[Crossref] [Google Scholar] [Pubmed]
- Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, et al. The International Registry of Acute Aortic Dissection (IRAD): New insights into an old disease. JAMA. 2000; 283(7): 897-903.
[Crossref] [Google Scholar] [Pubmed]
- Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014; 35(37): 2541-2619.
[Crossref] [Google Scholar] [Pubmed]
- JCS Joint Working Group. Guidelines for diagnosis and treatment of aortic aneurysm and aortic dissection (JCS 2011): Digest Version. Circ J. 2013; 77(3): 789-828.
[Crossref] [Google Scholar] [Pubmed]
- Nienaber CA, Clough RE. Management of acute aortic dissection. Lancet. 2015; 385(9970): 800-811.
[Crossref] [Google Scholar] [Pubmed]
- Bossone E, Suzuki T, Eagle KA, Weinsaft JW. Diagnosis of acute aortic syndromes. Herz. 2013; 38(3): 269-276.
[Crossref] [Google Scholar] [Pubmed]
- Siegal EM. Acute aortic dissection. J Hosp Med. 2006; 1(2): 94-105.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Mehran Gheshlaghi1, Mojgan Javedani Masroor2, Elahe Mohammadi1 and Hossein Sheibani3*2Shahid Akbar Abadi Clinical Research Development Unit (SACRDU), Iran University of Medical Sciences (IUMS), Tehran, Iran
3Department of Cardiology, Imam Hossein Hospital, Shahroud University of Medical Sciences, Shahroud, Iran
Citation: Gheshlaghi M: Primary Ventricular Fibrillation as the First Presentation of Aortic Dissection: A Case Report
Received: 15-Feb-2023 Accepted: 10-Mar-2023 Published: 17-Mar-2023, DOI: 10.31858/0975-8453.14.3.142-145
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3