Research - (2022) Volume 13, Issue 4
The Effectiveness of Aerobic Training (Walking) on the Functional Capacity of Heart Failure (HF) Patients: A Systematic Review
Siti Nurjannah1, Yuliana Syam2, Saldy Yusuf2, Aulia Insani Latif2, Safruddin Yahya3*, Asri3 and Muriyati3Abstract
This study aims to determine the effectiveness of Aerobic Training (AT) (walking) in increasing the functional capacity of HF patients. This study is a systematic review collected from 5 databases, namely PubMed, scienceDirect, Scopus, Wiley and proQuest. Articles meet the criteria for English language, publication of the last 10 years (2011-2020), and interventions focused on Aerobic Training (walking) in HF patients. A total of 7 articles met the criteria for Heart Failure patients, especially those with ejection fraction <40% and the New York Heart Association class II and III. Aerobic exercise intervention (walking) resulted in an increase in peak VO2 (mean differences: 1.7 ml/ kg/min, 3.7 ml/kg/min, 2 ml/kg/min, and 1.1 ml/kg/ min). In the 6-Minute walk there is an increase in the distance (average difference: 46.4 m, 98.3 m, 9 m, and 53.27 m). Duke Activity Status Index assessment, there is a significant change in p value 0.981. Also, in the Minnesota Living with Heart Failure questionnaire there was a clinical improvement (mean difference: 22.6 points, 19.7 points, and 2 points). The implementation of aerobic exercise (walking) with duration of 30-60 minutes for 3 times a week with low to moderate intensity training has been proven effective in increasing peak VO2, 6 minute walks, Duke Activity Status Index, and improving quality of life in Heart Failure patients.
Keywords
Walking exercise, Heart Failure (HF), Functional capacity
Introduction
The prevalence of Heart Failure (HF) will increase every year. It is estimated that it will increase by 46% from 2012 to 2030 by 8 million people aged ≥ 18 years (Go AS, etal., 2014). HF cases in the United States show an increase in prevalence from 5.7 million in 2012 to 6.2 million in 2016 (Virani SS, et al., 2020). In Asia, the prevalence of HF varies between 1.26% and 6.7%, and the mortality rate has been reported as 3.9%-6.7% (Mansouri A, et al., 2019). In Indonesia alone the prevalence of HF is reported to be 5% (Reyes EB, et al., 2016). Due to the high prevalence rate of HF, many previous studies were conducted to reduce readmission of HF patients but remain at high risk for hospitalization with 20% to 25% readmission within 30 days (Vargas J, et al., 2019). By reducing the re-admission of HF patients to hospitalization, an assessment of functional capacity is necessary.
Functional capacity is important in measuring the physical abilities of HF patients. Functional capacity is determined by the abil- ity to perform physical activities that require a certain level of aerobic capacity or skeletal muscle strength and endurance (Jurgens CY, et al., 2015). The functional status and general health tools used are peak VO2, Estimated Mets, Weber scale, 6-Minute walk, New York Heart Association (NYHA), Duke Activity Status Index (DASI), The Veterans Specific Activity Questionnaire (VSAQ), Kansas City Cardiomyopathy Questionnaire (KCCQ), and Minnesota Live with Heart Failure Questionnaire (MLHFQ) (Arena R, etal., 2007). This instrument has the advantage of being fast, cheap and safe (Arena R, etal., 2007). With the several advantages of this instrument, the modality of rehabilitation interventions in HF patients can be improved.
There are several modalities of rehabilitation interventions in HF patients to increase functional capacity. Aerobic Training (AT) is one of the core rehabilitation intervention modalities for patients with HF that has been shown to significantly improve exercise performance and functional capacity (Giallauria F, et al., 2018). Aerobic Training example: Walking is one of the most adopted intervention modalities in patients with HF and is recommended as initial activity (Giallauria F, et al., 2018). Walking is considered to be one of the most effective forms of physical activity, with little risk of injury among the low activity population, has been used as an intervention to reduce the burden of a number of chronic diseases including hypertension, cardiovascular risk, obesity, and osteoarthritis (Vetrovsky T, et al., 2017). Therefore, this review is expected to be an evidence-based reference for all health practi- tioners in providing AT recommendations, especially walking for patients with HF.
There needs to be a systematic review of AT (walking) interventions in HF patients. Recent meta-analysis studies suggest that resistance training in addition to standard HF drugs can provide clinically relevant improvements in exercise capacity and quality of life in Heart Failure with preserved Ejection Fraction (HFpEF) patients (Fukuta H, et al., 2016). However, further research is needed to establish the type, intensity, frequency, and duration in HFpEF patients (Fukuta H, etal., 2016). Likewise with other studies that explain that exercise provides a large increase in cardiopulmonary capacity because good functional capacity relieves symptoms and improves quality of life so it is attractive to the cardiac rehabilitation community (Giallauria F, et al., 2018). Further research should be designed to determine the best strategy in terms of type, duration, frequency and intensity of exercise programs (Giallauria F, et al., 2018). Therefore, the researcher conducted a systematic review of the literature in the form of a detailed summary of the type, intensity, frequency, and duration of exercise in a systematic review of AT (walking) on the functional capacity of HF patients. So the purpose of writing in this study is to identify the results of systematic literature analysis regarding the effectiveness of AT (walking) to increase the functional capacity of HF patients.
Methods
This systematic review uses the PRISMA Checklist 2009 guidelines (Moher D, et al., 2009).
Search strategyLiterature search was carried out in five data bases, namely PubMed, Sci- enceDirect, Scopus, Wiley, and ProQuest published from 2011 to 2020 and in English. The keywords use the PICO electronic method (Population, Intervention, Comparison and Outcome) (Aromataris E and Munn Z, 2020; Eriksen MB and Frandsen TF, 2018). The PICO in this article is P: “Heart Failure” or “Congestive heart failure”; I: “Walking” or “Walking exercise”; C: “Control” or “Usual care” and O: “Functional capacity” (Figure1).
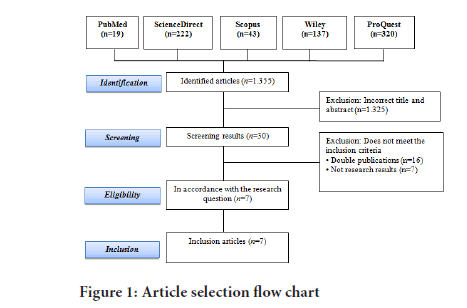
Figure 1: Article selection flow chart
Inclusion studiesThe selected studies were (1) HF patients aged>18 years; (2) focusing on AT (walking); (3) both control and usual care groups are described as maintaining the patient's usual/standard level of daily activity without a systematic exercise component including usual medical care, but may have received active interventions (eg: Education and psychological interven- tions); (4) functional capacity in the form of Peak VO2, Estimated Metabolic Equivalents (METs), Weber Scale, 6-Minute Walk, NYHA, DASI, VSAQ, KCCQ, and MLHFQ assessments; and (5) Randomized Control Trial (RCT) research design.
Exclusion studiesThe study was excluded if it met any of the following criteria: (1) patients with other cardiac diseases such as coronary artery disease, myocardial in- farction, chest angina, atrial fibrillation, peripheral artery disease, stroke, vascular disease, musculoskeletal disorders and pulmonary disease (2) review papers; and (3) study group intervention which had no comparison (Table 1).
| Researcher and year | Outcomes | Pre-intervention (Mean ± SD) | Post-intervention (Mean ± SD) | P value | Pre-control | Post-control | P value |
|---|---|---|---|---|---|---|---|
| Gary RA, et al., 2011 | 6-Minute walk | 364.3 ± 79.7 | 410.7 ± 91.5 | 0.006 | 306.6 ± 121.3 | 309.7 ± 135.4 | 0.855 |
| DASI | 49.2 ± 9.0 | 49.2 ± 6.9 | 0.981 | 45.8 ± 11.1 | 41.9 ± 10.1 | 0.146 | |
| MLHFQ | 56.1 ± 24.4 | 33.5 ± 22.9 | 0.001 | 49.8 ± 26.0 | 46.5 ± 19.7 | 0.547 | |
| Awotidebe TO, et al., 2016 | 6-Minute walk | 307.7 ± 22.5 | 406.0 ± 29.7 | 0.001* | 309.2 ± 27.8 | 321.0 ± 25.7 | 0.001* |
| Peak VO2 (mL/kg/min) | 8.6 ± 0.4 | 10.3 ± 0.5 | 0.001* | 8.6 ± 0.5 | 8.9 ± 0.4 | 0.001* | |
| Servantes DM, et al., 2012 | Peak VO2 (mL/kg/min) | 11.6 ± 2.1 | 15.3 ± 2.9 | <0.001* | 11.8 ± 2.1 | 9.6 ± 1.9 | <0.001* |
| MLHFQ | 40.4 ± 17.9 | 20.7 ± 16.3 | <0.001* | 46.5 ± 18.5 | 51.0 ± 16.8 | <0.001* | |
| Chien CL, et al., 2011 | 6-Minute walk (m) | 424 ± 145 | 433 ± 145 | Not written down | 432 ± 81 | 429 ± 93 | Not written down |
| MLHFQ | 11 ± 11 | 7 ± 9 | 16 ± 16 | 13 ± 13 | |||
| Lejczak A, et al., 2016 | Peak VO2 (mL/kg/min) | 9.2 | 11.2 | 0.05 | 9 | 14.5 | 0.05 |
| Safiyari-Hafizi H, et al., 2016 | Peak VO2 mL/kg/min | 10.1 ± 3.1 | 11.2 ± 2.9 | 0.040* | 10.1 ± 2.8 | 9.4 ± 2.4 | 0.040* |
| Teng HC, et al., 2018 | 6-Minute walk (m) | 295.38 ± 80.46 | 348.65 ± 78.51 | <0.001 | 265.03 ± 88.49 | 266.13 ± 81.61 | <0.001 |
Note: *Significance value between intervention and control groups. AT: Aerobic Training; HF: Heart Failure; DASI: Duke Activity Status Index; MLHFQ: Minnesota Live with Heart Failure Questionnaire
Table 1: Outcomes of AT (walking) articles on functional capacity of HF patients
Risk of bias assessment
Article selection was assessed using 2 instruments, namely Critical Appraisal Skill Program (CASP) in 2018 and CEBM (Center for Evidence-Based Medicine, 2014). In addition, the quality of the articles was filtered and assessed effectively using the Cochrane Risk of Bias Tool recommended by the Cochrane Handbook for Systematic Review. This tool consists of six items, namely random allocation, allocation of sample concealment, blinding, incomplete results, selective result reporting and other sources of potential bias. Each item is rated "yes (+)" "no (-)" or "unclear (?)". According to the Cochrane Handbook and previous studies, test quality can be divided into 3 levels. Level A if the article fully meets all 6 criteria. Level B is defined when 1 or more criteria are partially met and are considered low risk of bias. Meanwhile, if 1 or more criteria are not met, it is called level C which is considered to have a high risk of bias (Higgins JP, etal., 2011) (Table 2).
| Study and Country | Random sequence generation | Allocation concealment | Blinding of participants | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Levels |
|---|---|---|---|---|---|---|---|
| Gary RA, et al., 2011 | + | + | ? | - | + | + | B |
| Awotidebe TO, et al., 2016 | + | + | + | + | + | + | A |
| Servantes DM, et al., 2012 | + | + | + | + | + | + | A |
| Chien CL, et al., 2011 | + | + | - | ? | + | + | B |
| Safiyari-Hafizi H, et al., 2016 | + | + | ? | + | + | + | B |
| Lejczak A, et al., 2016 | + | + | ? | ? | + | + | B |
| Teng HC, et al., 2018 | + | + | - | - | + | + | C |
Table 2: Risk of bias
Data extraction
Presentation of data from studies that have entered into the final results, will be extracted then made in a narrative form and presented in a data table consisting of researchers, countries, research objectives, characteristics of research samples, research interventions, research control, types of aspects measured, and results researchs.
Results
From the initial literature search, 1,355 published articles were identified, after screening for unsuitable titles and abstracts, 1,325 articles were excluded. Among the remaining 30 trials, 23 studies were excluded for the following reasons: Double publication (n=16) and not study results (n=7). Thus, a total of 7 studies were included in the final analysis (Awotidebe TO, et al., 2016; Servantes DM, et al., 2012; Gary RA, et al., 2011; Chien CL, et al., 2011; Safiyari-Hafizi H, et al., 2016; Lejczak A, et al., 2016; Teng HC, et al., 2018)
Research design
The articles that have been summarized are 7 articles using the RCT research design, each of which was conducted in the USA, Nigeria, Brazil, Taiwan (n=2), Poland and Columbia.
Risk of bias
The overall risk of bias from the included studies was rated moderate because only 2 articles fully met all 6 criteria of the assessment recommended by the Cochrane Handbook for Systematic Review (Awotidebe TO, et al., 2016; Servantes DM, etal., 2012). There are 4 articles with partially fulfilled criteria, namely one or more criteria are met and are considered low risk of bias (Gary RA, etal., 2011; Chien CL, etal., 2011; Safiyari-Hafizi H, etal., 2016; Lejczak A, etal., 2016), and one article has a high risk of bias because one or more of the criteria are not met which is considered to have a high risk of bias (Teng HC, etal., 2018) (Table2).
Characteristics of the research sample
Of the 7 articles that were included, the sample size in the study was 24 male and female samples aged 40-75 years (Gary RA, etal., 2011). There are 70 samples aged ≥ 50 years, mostly female (Awotidebe TO, etal., 2016). Meanwhile, there are 50 samples aged 30-70 years, the average is female (Servantes DM, etal., 2012). Next, 51 samples with a mean age of 58 years were male (Chien CL, etal., 2011). There were 24 samples with an average age of 30-63 years, all samples were male (Lejczak A, etal., 2016). Furthermore, 40 samples aged <75 years (Safiyari-Hafizi H, etal., 2016). The study amounted to 90 samples aged ≥ 20 years, mostly male (Teng HC, et al., 2018).
Type of exercise
Most of the types of exercises from the seven articles are AT (walking)+Strength Training (ST) (Awotidebe TO, etal., 2016; Servantes DM, etal., 2012; Chien CL, etal., 2011; Safiyari-Hafizi H, etal., 2016). There is one study doing a combined type of AT (walking) exercise+resistance exercise (Gary RA, etal., 2011), types of Nordic walking exercises (Lejczak A, etal., 2016) and the last type of exercise with WEB intervention (Teng HC, et al., 2018).
Exercise duration
Exercise duration of 30-60 minutes was mostly done in research (Awotidebe TO, etal., 2016; Servantes DM, etal., 2012; Gary RA, etal., 2011; Chien CL, etal., 2011). The training duration of each interval varies and is adjusted individually depending on their functional capacity to ensure safety and program progress (Safiyari-Hafizi H, etal., 2016). Furthermore, the duration of the exercise starts with a 5-minute warm-up, 15-minute WEB, and 5-minute cooling (Teng HC, etal., 2018).
Exercise frequency
The frequency of exercise 3 times a week was the most used in the study (Awotidebe TO, etal., 2016; Gary RA, etal., 2011; Chien CL, etal., 2011).
Another study said that the frequency of exercise is adjusted regularly according to patient capacity and according to changes in heart rate response to exercise (Safiyari-Hafizi H, et al., 2016). Furthermore, the frequency of exercise is done 2 times a day in the morning and evening (Teng HC, et al., 2018).
Exercise intensity
Low-moderate intensity exercises are often performed in studies (Gary RA, etal., 2011; Chien CL, etal., 2011). Doing exercise intensity ranges from 60%-70% of the maximum heart (Awotidebe TO, et al., 2016). Furthermore, another study conducted exercise intensity which was de- termined by the heart rate associated with anaerobic threshold (VO2AT) (Servantes DM, etal ., 2012). There is also high intensity exercise (80%-85% peak VO2) followed by an active recovery period (40%-50% peak VO2) (Safiyari-Hafizi H, etal., 2016).
Peak VO2
A more significant increase in oxygen volume (VO2) max 1.7 ml/kg/min with a significant p value of 0.001 (Awotidebe TO, etal., 2016). There was a significant increase in both interventions at peak values of VO2 and VO2 AT with the addition of 5.2 and 3.7 ml/kg/min and 5.3 and 3.5 ml/kg/min, respectively with p value<0.001 (Servantes DM, etal., 2012). The study states that the VO2 value increases significantly with the addition of 2 ml / kg / min value with p value<0.005 (Lejczak A, et al., 2016). Also, the addition of the VO2 value was significantly 1.1 ml/kg/min with a p value of 0.040 (Safiyari-Hafizi H, etal., 2016).
6-Minute walk
6-Minute walk increases an additional distance of 46.4 meters with a significance p value of 0.006 (Gary RA, et al., 2011). The research shows that the increase in the 6-minute walk distance is 98.3 meters with a significance p value of 0.001 (Awotidebe TO, etal., 2016). Other research says that the 6-minute walk increases the distance traveled by 9 meters and 1% predicted (Chien CL, etal., 2011). The additional distance in the 6-minute walk with a significance p value<0.005 (Safiyari-Hafizi H, etal., 2016). The study states that the additional 6-minute walk distance is significantly 56.27 meters with a p value of 0.001 (Teng HC, et al., 2018).
Duke Activity Status Index (DASI)
The intervention group for DASI, from pre intervention 49.2 ± 9.0 and post intervention 49.2 ± 6.9 with a significance value of p value 0.981(Gary RA, et al., 2011).
Minnesota Live with Heart Failure Questionnaire (MLHFQ)
Improved quality of life for MLHFQ was seen pre intervention 56.1 ± 24.4 and post intervention 33.5 ± 22.9 with a significance value of p value 0.001 (Gary RA, etal., 2011). In the study, it was seen that MLHFQ pre intervention 40.4 ± 17.9 and post intervention 20.7 ± 16.3 with a significance value of p value<0.001 (Servantes DM, etal., 2012). Meanwhile, for pre intervention MLHFQ 11 ± 11 and 7 ± 9 post intervention (Chien CL, etal., 2011). Furthermore, the study stated that improved Quality of Life (QoL) and few adverse symptoms during exercise were seen for MLHFQ with a significance value of p value<0.005 (Safiyari-Hafizi H, etal., 2016) (Table2).
Discussion
The average sample size is 24 to 50 samples. The power of an intervention will increase with a larger sample (White H, et al., 2014). A sample size that is too small would have insufficient power to detect true differences, so that significant differences between study groups may not be statistically significant (Malone HE, et al., 2016). So from the results of a literature review, a sample size of 24 to 50 samples shows the power of an intervention.
Performing AT interventions (walking)
The type of training that combines AT (walking) and Strength Training is the most widely used. This is consistent with research that the AT program and combined resistance training are effective in increasing VO2 peak, muscle strength, 6-minute walk, and quality of life in HF patients (Wang Z, et al., 2019). Other studies have also shown that resistance training increases muscle strength, Health-Related Quality of Life (HRQOL) and peak VO2 (even in small amounts) (Gomes-Neto M, et al., 2019). Therefore, joint training in the form of AT (walking) with Strength Training can maintain and increase muscle strength and functional ability.
The most widely used duration is 30-60 minutes. This is consistent with previous research saying that exercise usually involves walking for 30-60 minutes to achieve a peak VO2 oxygen uptake of 40%-80% (Xie B, et al., 2017). uration of exercise for 30 minutes or 60 minutes will increase the elasticity of the arteries and produce minimal oxidant stress (O’Keefe JH, et al., 2014). If more than 60 minutes per session can cause increased oxidant stress in the blood vessels to become stiff, especially among men over 50 years of age (O’Keefe JH, et al., 2014). Therefore, walking is done for at least 30-60 minutes because it increases the elasticity of the arteries and results in minimal oxidant stress.
The frequency of exercise is carried out 3 times a week. This is consistent with other studies that count 1 to 2.4 hours of exercise for 2 to 3 times per week as a standard for optimal quantity and frequency of aerobic exercise to improve health (Patel H, etal., 2017). Other studies have also suggested that those who are moderately active (2 to 4 times per week) are the levels of physical activity that appear to provide the greatest benefit in terms of survival (Mons U, etal., 2014). Thus, walking exercises performed 3 times a week serve as the standard for optimal quantity and frequency of exercise to improve health and provide the greatest benefit in terms of survival.
The most widely used low-moderate intensity exercise in this study. This is in line with studies consistently showing that moderate-intensity physical activity is beneficial for long-term cardiovascular health (O’Keefe JH, et al., 2014). Likewise, a prospective observational study of older men and women (mean age 73 years) reported that moderate-intensity physical activity such as walking reduced the risk of heart rhythm disorders by about a third (O’Keefe JH, et al., 2014). Thus, moderate low intensity exercise can improve cardiovascular prognosis and reduce the risk of heart rhythm disturbances.
Results of the effectiveness AT interventions (walking)In this study, there was a more significant improvement with increasing peak VO2. This is in line with previous research that training-induced increases in peak VO2 could have a beneficial effect on clinical outcomes (Giallauria F, et al., 2018). From a clinical point of view, regular exercise may be beneficial in HF patients even though it does not significantly increase VO2 peaks but reduces/prevents decreases in VO2 peaks exacer- bated by sedentary lifestyle (Mandic S, et al., 2009). Thus, walking can in- crease the peak VO2 which is sufficient to meet the body's metabolic needs in increasing the patient's functional capacity.
Likewise, with an increase in the 6-Minute walk distance. This is in line with research that states that the 6-minute walk as a measure of functional capacity has been used as a screening tool in HF (<300 meters) and can be a useful tool for assessing weakness which is a significant risk marker and potential contraindication to non-strategy pharmacological in HF (Crespo‐Leiro MG, et al., 2018). Thus, the 6-minute walk serves as a useful screening tool to assess weakness in HF patients.
In addition to the 6-Minute walk there is also an increase in the DASI assessment. The tie is especially useful for those whose walking speed is affected by musculoskeletal problems but maintains a high level of regular physical activity (Potter E, etal., 2020). In particular, the reduction in DASI predicts short to medium term progression to real HF with a symptom state that should be considered HF (Potter E, etal., 2020). Thus, measurement of DASI could be of benefit to patients with HF in terms of response to increased functional capacity.
In this study, there was an improvement in quality of life and few adverse symptoms during exercise were seen in MLHFQ. This is consistent with previous studies that interventions such as exercise can improve quality of life and also reduce the incidence of death in patients with HF (Wu JR, etal., 2016). Previous studies have also shown that significant reductions in MLHFQ scores can be achieved well after exercise with a 5 point reduction considered clinically relevant which suggests that short-term cardiac rehabilitation is also beneficial and that some patients experience appreciable positive changes in physical and emotional quality of life (Beale L, etal., 2013). Therefore, AT (walking) can improve the quality of life.
This study has several limitations. This study only focuses on the RCT design so that the number of articles obtained is small (limited). Because the number of randomized controlled studies is small, publication bias is unavoidable and the results should be interpreted with caution. Patients in the study may have engaged in some covert physical activity that was not monitored during the study. Some of the participants who refused to attend the outcome assessment tended to have high levels of anxiety and depression and thus require additional strategies to reduce anxiety and de- pression in response to clinical research compliance. Further studies may be needed to carry out monitoring or surveillance of physical activity and explore the relationship between psychological status, physical function, and quality of life in HF patients.
Conclusion
AT intervention (walking) is a common activity, is always done in daily activities, and has long been recommended by researchers to increase the functional capacity of HF patients in research. The results of the effectiveness of AT interventions (walking) were that there was a more significant improvement in VO2 peaks, an increase in the additional mileage on 6 minute walks, improved DASI assessments, and improved quality of life.
References
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics-2014 update: A report from the American Heart Association. Circulation. 2014; 129(3): 28-92.
[Crossref] [Google Scholar] [Pubmed]
- Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: A report from the American Heart Association. Circulation. 2020; 141(9): 139-596.
[Crossref] [Google Scholar] [Pubmed]
- Mansouri A, Baraz S, Elahi N, Malehi AS, Saberipour B. The effect of an educational program based on Roy's adaptation model on the quality of life of patients suffering from heart failure: A clinical trial study. Jpn J Nurs Sci. 2019; 16(4): 459-467.
[Crossref] [Google Scholar] [Pubmed]
- Reyes EB, Ha JW, Firdaus I, Ghazi AM, Phrommintikul A, Sim D, et al. Heart failure across Asia: Same healthcare burden but differences in organization of care. Int J Cardiol. 2016; 223: 163-167.
[Crossref] [Google Scholar] [Pubmed]
- Vargas J, Goel A, Stoner T, Fowler K. Heart failure hospitalist can reduce length of stay, can reduce readmission, and can reduce cost. J Card Fail. 2019; 25(8): 121.
- Jurgens CY, Goodlin S, Dolansky M, Ahmed A, Fonarow GC, Boxer R, et al. Heart failure management in skilled nursing facilities: A scientific statement from the American Heart Association and the Heart Failure Society of America. Circ Heart Fail. 2015; 8(3): 655-687.
[Crossref] [Google Scholar] [Pubmed]
- Arena R, Myers J, Williams MA, Gulati M, Kligfield P, Balady GJ, et al. Assessment of functional capacity in clinical and research settings: A scientific statement from the American Heart Association Committee on Exercise, Rehabilitation, and Prevention of the Council on Clinical Cardiology and the Council on Cardiovascular Nursing. Circulation. 2007; 116(3): 329-343.
[Crossref] [Google Scholar] [Pubmed]
- Giallauria F, Piccioli L, Vitale G, Sarullo FM. Exercise training in patients with chronic heart failure: A new challenge for cardiac rehabilitation community. Monaldi Arch Chest Dis. 2018; 88(3).
[Crossref] [Google Scholar] [Pubmed]
- Vetrovsky T, Siranec M, Parenica J, Griva M, Stastny J, Precek J, et al. Effect of a 6-month pedometer-based walking intervention on functional capacity in patients with chronic heart failure with reduced (HFrEF) and with preserved (HFpEF) ejection fraction: Study protocol for two multicenter randomized controlled trials. J Transl Med. 2017; 15(1): 1-10.
[Crossref] [Google Scholar] [Pubmed]
- Fukuta H, Goto T, Wakami K, Ohte N. Effects of drug and exercise intervention on functional capacity and quality of life in heart failure with preserved ejection fraction: A meta-analysis of randomized controlled trials. Eur J Prev Cardiol. 2016; 23(1): 78-85.
[Crossref] [Google Scholar] [Pubmed]
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009; 6(4): e1000097.
[Crossref] [Google Scholar] [Pubmed]
- Aromataris E, Munn Z. Chapter 1 : Systematic Review. Joanna Briggs Institute Reviewer’s Manual. 2020; 6: 74-82.
- Eriksen MB, Frandsen TF. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: A systematic review. J Med Libr Assoc. 2018; 106(4): 420.
[Crossref] [Google Scholar] [Pubmed]
- CEBMa. Critical appraisal of a case study: Appraisal questions. Center for Evidence-Based Management (CEBMa). 2014.
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011; 343.
[Crossref] [Google Scholar] [Pubmed]
- Awotidebe TO, Adedoyin RA, Balogun MO, Adebayo RA, Adeyeye VO, Oke KI, et al. Effects of cardiac rehabilitation exercise protocols on physical function in patients with chronic heart failure: An experience from a resource constraint nation. Int J Clin Med. 2016; 7(8): 547-557.
- Servantes DM, Pelcerman A, Salvetti XM, Salles AF, de Albuquerque PF, de Salles FC, et al. Effects of home-based exercise training for patients with chronic heart failure and sleep apnoea: A randomized comparison of two different programmes. Clin Rehabil. 2012; 26(1): 45-57.
[Crossref] [Google Scholar] [Pubmed]
- Gary RA, Cress ME, Higgins MK, Smith AL, Dunbar SB. Combined aerobic and resistance exercise program improves task performance in patients with heart failure. Arch Phys Med Rehabil. 2011; 92(9): 1371-1381.
[Crossref] [Google Scholar] [Pubmed]
- Chien CL, Lee CM, Wu YW, Wu YT. Home-based exercise improves the quality of life and physical function but not the psychological status of people with chronic heart failure: A randomised trial. J Physiother. 2011; 57(3): 157-163.
[Crossref] [Google Scholar] [Pubmed]
- Safiyari-Hafizi H, Taunton J, Ignaszewski A, Warburton DE. The health benefits of a 12-week home-based interval training cardiac rehabilitation program in patients with heart failure. Can J Cardiol. 2016; 32(4): 561-567.
[Crossref] [Google Scholar] [Pubmed]
- Lejczak A, Josiak K, Węgrzynowska-Teodorczyk K, Rudzińska E, Jankowska EA, Banasiak W, et al. Nordic walking may safely increase the intensity of exercise training in healthy subjects and in patients with chronic heart failure. Adv Clin Exp Med. 2016; 25(1): 145-149.
[Crossref] [Google Scholar] [Pubmed]
- Teng HC, Yeh ML, Wang MH. Walking with controlled breathing improves exercise tolerance, anxiety, and quality of life in heart failure patients: A randomized controlled trial. Eur J Cardiovasc Nurs. 2018; 17(8): 717-727.
[Crossref] [Google Scholar] [Pubmed]
- White H, Sabarwal S, de Hoop T. Randomized Controlled Trials (RCTs). Methodological Briefs, Impact Evaluation. 2014.
- Malone HE, Nicholl H, Coyne I. Fundamentals of estimating sample size. Nurse Res. 2016; 23(5).
[Crossref] [Google Scholar] [Pubmed]
- Wang Z, Peng X, Li K, Wu CJ. Effects of combined aerobic and resistance training in patients with heart failure: A meta‐analysis of randomized, controlled trials. Nurs Health Sci. 2019; 21(2): 148-156.
[Crossref] [Google Scholar] [Pubmed]
- Gomes-Neto M, Duraes AR, Conceição LS, Roever L, Silva CM, Alves IG, et al. Effect of combined aerobic and resistance training on peak oxygen consumption, muscle strength and health-related quality of life in patients with heart failure with reduced left ventricular ejection fraction: A systematic review and meta-analysis. Int J Cardiol. 2019; 293: 165-175.
[Crossref] [Google Scholar] [Pubmed]
- Xie B, Yan X, Cai X, Li J. Effects of high-intensity interval training on aerobic capacity in cardiac patients: A systematic review with meta-analysis. Biomed Res Int. 2017.
[Crossref] [Google Scholar] [Pubmed]
- O’Keefe JH, Franklin B, Lavie CJ. Exercising for health and longevity vs. peak performance: Different regimens for different goals. Mayo Clin Proc. 2014; 89(9): 1171-1175.
[Crossref] [Google Scholar] [Pubmed]
- Patel H, Alkhawam H, Madanieh R, Shah N, Kosmas CE, Vittorio TJ. Aerobic vs. anaerobic exercise training effects on the cardiovascular system. World J Cardiol. 2017; 9(2): 134.
[Crossref] [Google Scholar] [Pubmed]
- Mons U, Hahmann H, Brenner H. A reverse J-shaped association of leisure time physical activity with prognosis in patients with stable coronary heart disease: Evidence from a large cohort with repeated measurements. Heart. 2014; 100(13): 1043-1049.
[Crossref] [Google Scholar] [Pubmed]
- Mandic S, Tymchak W, Kim D, Daub B, Quinney HA, Taylor D, et al. Effects of aerobic or aerobic and resistance training on cardiorespiratory and skeletal muscle function in heart failure: A randomized controlled pilot trial. Clin Rehabil. 2009; 23(3): 207-216.
[Crossref] [Google Scholar] [Pubmed]
- Crespo‐Leiro MG, Metra M, Lund LH, Milicic D, Costanzo MR, Filippatos G, et al. Advanced heart failure: A position statement of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2018; 20(11): 1505-1535.
[Crossref] [Google Scholar] [Pubmed]
- Potter E, Yang H, Wright L, Wang B, Marwick TH. Measurement of functional capacity to discriminate clinical from subclinical heart failure in patients ≥ 65 years of age. Am J Cardiol. 2020; 127: 84-91.
[Crossref] [Google Scholar] [Pubmed]
- Wu JR, Lennie TA, Frazier SK, Moser DK. Health-related quality of life, functional status and cardiac event-free survival in patients with heart failure. J Cardiovasc Nurs. 2016; 31(3): 236.
[Crossref] [Google Scholar] [Pubmed]
- Beale L, McIntosh R, Raju P, Guy L, Brickley G. A comparison of high intensity interval training with circuit training in a short-term cardiac rehabilitation programme for patients with chronic heart failure. Int J Phys Med Rehabil. 2013; 1(6): 1-7.
Author Info
Siti Nurjannah1, Yuliana Syam2, Saldy Yusuf2, Aulia Insani Latif2, Safruddin Yahya3*, Asri3 and Muriyati32Department of Nursing, Hasanuddin University, Makassar, Indonesia
3Department of Nursing, STIKES Panrita Husada, Bulukumba, Indonesia
Citation: Nurjannah S: The Effectiveness of Aerobic Training (Walking) on the Functional Capacity of Heart Failure (HF) Patients: A Systematic Review
Received: 08-Mar-2022 Accepted: 29-Mar-2022 Published: 05-Apr-2022, DOI: 10.31858/0975-8453.13.4.273-278
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






