Review Article - (2023) Volume 14, Issue 9
Abstract
Topical corticosteroids are potent preferable drug of choice in dermatology, but its abuse and misuse are increasing. People tend to use topical corticosteroids for instant relief from itching and rashes but it may cause other local side effects. There is a misuse of topical corticosteroids due to number of reasons like easy availability as over the counter, available at affordable price, faster relief and onset of action. Long term use may cause systemic and topical side effects like skin atrophy, striae and telangiectasia. Prescribing these agents should be done cautiously and dermatologist should take time to explain patient on rational use of these agents-use, duration, dosage, frequency and side effects. Without any lesion or without any advice from dermatologist people use these agents irrationally for skin lightening, skin pigmentation. These practices should not be promoted and strict regulations should be taken to reduce misuse of topical corticosteroids. There should be an evidence based prescribing guidelines to prevent further abuse of these agents.
Keywords
Topical corticosteroids, Clinical pharmacist, Steroid use and misuse, Adverse effects
Introduction
In modern practice, steroids are used in medicine, dermatology, cosmetology, rheumatology etc. and their use is increasing, we are aware of steroid induced side effects. Increasing use of topical steroids is due to its unique impact on physiology that includes faster action and relief, multiple indications in wide variety of dermatological conditions like atopic dermatitis, psoriasis, lichen planus, immunobullous disorder etc.
• Drug based-Due to its potency and faster relief of inflammation, multiple indication, drug availability and Fixed Dose Combination (FDC) with antimicrobials.
• Patient based-Women use TCS for skin pigmentation and for beautification.
• Prescriber based-Prescribing of potent TCS for simple dermatoses.
The side effects of these agents range from mild to very severe depending on body surface area being exposed, duration of exposure and frequency of usage. Eventually long-term exposure to these agents may causes side effects that are serious and unneglectable. It is found that soft, sensitive areas like face and genitals with a high rate of transcutaneous absorption and high vascularity will have more side effects (Al Dhafiri M, et al., 2022). Other leading causes for Topical Corticosteroids (TCS) abuse maybe due to its easy availability in Indian market as OTC and poor access to dermatologist in rural community (Kumar S, et al., 2016). Other cause for TCS abuse may include its easy compatibility with other agents like antibiotics, antifungal and depigmenting agents. Recently, a study done at Rural Tertiary Care Teaching Hospital in Maharashtra, India concluded that 28% of 500 prescriptions had TCS, out of which 98% were very potent corticosteroids; and in 85% of cases, the basis of prescribing TCS could not be established (Kakroo SN and Beg MA, 2018). That was an alarming situation where topical steroids are prescribed irrationally, inappropriately without Food and Drug Administration (FDA) indication, and starting topical steroid therapy with potent class (Figure 1).
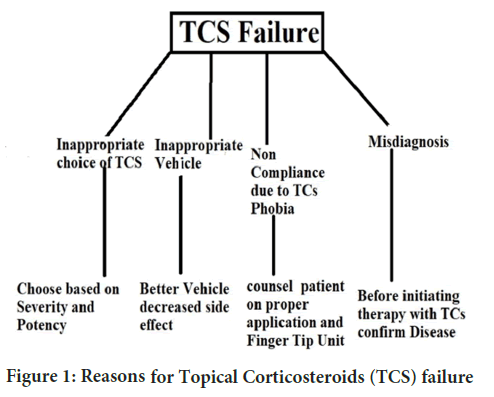
Figure 1: Reasons for Topical Corticosteroids (TCS) failure
Literature Review
Reasons for wide use of TCS in India
Two distinct ends of topical TCS are steroid phobia and steroid abuse both leading to treatment failure or under therapy (Das A and Panda S, 2017). Corticosteroids from the time of discovery it is well known that they can cause systemic and topical side effects when they are administered by oral or parenteral route. Some of systemic side effects include weight gain, hypertension, cushingoid habitus, osteopenia, and hirsutism. Ocular side effects such as glaucoma and cataract are commonly seen in paediatric (Jinagal J, et al., 2019). Locally it can cause immediate effects as burning and stinging and long-term use may cause skin atrophy, hypo/hyper pigmentation, photosensitivity, premature ageing of skin due to loss of skin barriers. TCS withdrawal can be divided into two distinct morphologic syndromes: Papulopustular and erythema oedematous. Erythematoedematous type is more frequent in patients who have chronic dermatoses such as atopic dermatitis and seborrheic dermatitis and it is characterized by redness, scaling, wheel formation with or without burning sensation papulopustular type is more common in patients who are using TCS for pigmentary disorders or acneiform conditions. The papulopustular withdrawal subtype is more likely in patients who develop steroid rosacea. The papulopustular variant can be differentiated from the erythema oedematous subtype by the prominent features of pustules and papules, along with erythema, but less frequently swelling, oedema, burning, and stinging (Hajar T, et al., 2015). The adverse reactions are strongly associated potency of topical corticosteroids used and have increased in frequency of adverse reactions with the introduction of high potency topical corticosteroids (Dhar S, et al., 2014).
To prevent the rebound, consider discontinuation of the treatment, with the use of a less potent preparation and/or the use of an emollient vehicle alternately (Rathi SK and D’Souza P, 2012). If these agents are used appropriately and rationally, they are safe and seem to have lesser side effects and withdrawal symptoms. According to recent guidelines it is recommended to use high dose corticosteroids during the acute flares and continue with lowest possible dose corticosteroid when the episode is under control. Women are subjected to steroid abuse hence depending on severity of dermatoses one should use TCs of the least potency required and the duration and amount should be monitored judiciously. The risk of adverse events is more in area of application where there is high absorption that includes genitals, eyelids, skin fold, armpits and vulva. In body sites with thin skin (face, eyelids, scrotum and flexures), milder corticosteroids should be used and also in dermatoses involving extensive body surface areas and in children; such practice is meant to reduce therapy-related side effects (Mehta AB, et al., 2016).
Potency of TCS
• Patient: Based on patient age (Infant child or adult).
• Lesion location: Less vascular or more vascular.
• Lesion type and severity: Size and numbers of lesions.
• Topical medication: Molecular structure, percentage, formulation, and vehicle.
TCS prescribing guidelines
Prescribe the correct class: The weakest steroid that controls the disease effectively should be chosen to reduce the risk of topical steroid withdrawal reactions. Initially, topical steroids should be applied once daily, if no benefit is seen after 7-10 days, change to twice daily for a further 7-10 day.
Prescribe the correct amount: Explain to patient how to apply just a small amount and rub gently into the skin until it disappears. Prescriber/Pharmacist should educate patient on rational application of these topical agent and patient should be assured on specific Fingertip Unit (FTU) for each area of application.
Reassure the patient response:
• Many patients fear TCS
• Incorrect diagnosis
• Patient who keeps using the medication beyond the prescribed duration to prevent reoccurrence.
Prefer non-steroidal cream whenever appropriate: TCS+Moisturizing cream is found to be efficient than single TCS.
Minimize topical side effect in a best possible way: Acne and perioral dermatitis: Educate patient avoid touching their face after applying their medication. Skin atrophy: The loss of the collagen that supports the arteries causes telangiectasia and easy bruising (Murray E, 2019; NIF, 2023).
Steps in prescribing TCS:
• Make a diagnosis.
• Choose an appropriate agent by considering area of application, severity and go for least potent agent for short duration of time.
• Plan a therapeutic goal-Duration of application, appropriate vehicle and body surface area to be applied.
• Counsel patient-Rational use of these agents, fingertip unit and dosage and frequency.
• Monitor patient-Monitor whether treatment goal is achieved; look for both beneficial and harmful effects.
• Reassure-Switch to stronger agents if needed, if misdiagnosed-reassure diagnosis
Discussion
Misuse of TC, which is defined as inappropriate topical steroid usage on the skin due to improper formulation, frequency, duration, or indications applied for specific skin disorders (Mahar S, et al., 2016). Misuse of topical steroids are increasing with the occurrence of acute and chronic adverse effect, there should be a stewardship and proper prescribing guidelines. Dermatologist, Physicians and pharmacist are mainly attributed for TCS abuse followed by friends, family members etc., to the extent that they ignored to inform the patients about the risks and proper dosage of topical corticosteroids (Dey VK, 2014). An Australian survey found that 36% of pharmacists under recognized nonadherence as a reason for treatment failure (Su JC, et al., 2021). It was observed that majority of patients were ignorant about side effects, dosage and mode of application. Another major issue happening in clinics and hospitals are use of potent TCS over mild and moderate anticipating faster outcome. In a study conducted in Kerala, it was found more than 50.78% of total number of steroid prescribed belongs to very potent category, followed by 4.32% were mild, 12.19% and 32.67% were moderate and potent steroids respectively (Abraham MS, et al., 2016). Other trend seen in Indian population is using TCS without any dermatoses. There was a study in China which depicted that 28.5% used steroids on the face without any underlying dermatosis (Lu H, et al., 2010) and there was a similar study carried out in rural tertiary hospital India where 74% people used topical corticosteroids without any indication (Sinha A, et al., 2016).
Educating patient about indication of each prescription and duration is important in preventing adverse effect to a certain extent. Type of disease and area of applications are two factors that decides dosage and Fingertip Unit (FTU), so proper education should be made among patients on appropriate application of these topical agents. In the study, they have also found that frequency and duration of treatment were also not mentioned in some of prescriptions that can directly lead to an increase in the financial burden to the patients followed by therapeutic failure or toxicity. It is crucial that the doctor selects the best medication for the patient, at a price that is affordable and will provide relief to the patient. It is essential to spend more time with the patient in explaining the dosing and the adverse effects associated with self-medication of the same drug. However, physicians are more likely to prescribe more generic medications. It would however be encouraging to have more generic prescribing. Despite the increased likelihood that a Fixed Dose Combination (FDC) containing a corticosteroid would be prescribed, it is necessary to prescribe them as single preparations as the adverse effects associated with their use are more in fixed (Abraham MS, et al., 2016). In another study, they found out that none of the patients were aware of the dose and how much of the drug should be applied to specific body surface area (Sheth NK and Nair PA, 2021).
Women population are more likely to get affected by adverse effects of TCS due to number of reasons like inappropriate use as cosmetics and beautifying agents. In a survey on 769 women in Saudi, 30.3% of the patients were in age group of 31 to 40 years, most of them used topical steroids for skin lightning and to reduce skin wrinkles and ageing (Shumoukh SA, et al., 2019). In a study, 6723 patients it was found that 379 (5.63%) had experienced an adverse effect due to misuse of these agents, 78.89% of them were women. Out of it More than 65% of the patients were grouped in the age group of 10-29 years. Only 3.43% of patients were aware of topical corticosteroids side effects. Patients are unaware of dose, dosage and frequency. People seems to reuse the prescriptions for new lesion and rashes considering it similar to other chronic diseases like diabetics, epilepsy. And also, there is a malpractice that friends and relatives suggesting branded agents to treat similar looking skin problems (Rathi SK and D’Souza P, 2012). In a study by Mahar S, et al. 97.6% did not know the dosage i.e., how much amount of the drug (Fingertip Unit) should be applied to specific body area. One patient followed the pharmacist’s advice and applied 5 tubes of topical steroid within a week. A total of 34% patients inappropriately used the TC in terms of incorrect frequency. In this study it is found that dermatologists contributed only 4.45% to the prescription. Since they don’t write the necessary recommendations for the exact duration, dose, and amount to be administered, dermatologists are therefore also responsible for the misuse of TC. Proper awareness should be raised among dermatologists regarding rational use of topical steroids.
In rural areas of our country where dermatologist to patient ratio is very low, patient’s primary contact for any health-related problem is chemist and pharmacist. The central and state drug regulatory body should sensitize these personals on topical corticosteroids, its rational use and adverse effects. Patient should be properly counselled on dose, frequency, site of application and duration. Initially TCs can bring a faster relief to patient as these agents reduce inflammation but in long term use can flare up rebound withdrawal symptoms. Finally, patient should be educated properly in outpatient setting and over the counter on rational use of these agents. These issue, although reported from many places worldwide it has wide significant impact in our country where there are just a few dermatologists to treat such a huge population and there are no strict regulations for Over- the-Counter (OTC) prescription of these drugs (Mahar S, et al., 2016). In another study, it was found that the pharmacists and paramedical personnel to be held accountable for the abuse of topical corticosteroids along with the patient, friends or family. It is the role and responsibility of general physicians and dermatologist that they have to bring to the notice of patient concerning the possible side effects and proper dosing of topical corticosteroids. Pharmacists tend to dispense these topical agents based on prior knowledge and experience which may be irrational. An evidence based medical practice should be initiated in OPD and OTC. Pharmacists in chemist shop and medical shops, whose qualification is not known, they play as doctors doling out advice about which TCS to use. These potent types of TCS are readily available at reasonable price, which has led to widespread usage that had a number of negative impacts. Despite being a severe problem, the misuse of TC products in India has only been the subject of a few numbers of researches (Mahar S, et al., 2016).
Factors decreasing TCS harm:
• Patient factors include early visit to physicians and treatment, medication adherence, life style, mental and social wellbeing.
• Prescriber factor include proper selection potency, appropriate vehicle and rational regimen.
• Pharmacist factor include patient education and awareness, methods to improve medication adherence.
Factors increasing/pre disposing to TCS harm:
Patient factors includes late visit to physician, use of TCS beyond indication, using for new rashes or lesion without advice from dermatologist, using for non dermatoses reasons like fairness and beautifying, using TCS from OTC.• Prescriber factors include lack of information on TCS, its potency, its vehicle, no proper guidelines for prescribing.
• Pharmacist factors include lack of patient education and awareness, unqualified person prescribing Topical agents like chemist, pharmacist, friends and relatives.
Conclusion
Topical corticosteroids are a drug of choice for many dermatologists for acute and chronic dermatoses. On long term use, these agents may bring some serious adverse effects ranging from systemically Hypothalamic Pituitary Adrenal Axis Suppression (HPAAS) to locally causing atrophy, striae rosea, telangiectasia, purpura erythroderma. Even though many serious systemic and topical adverse effects have been identified very few quality studies have been done on safety and efficacy of these agents. Easy availability at affordable price in Indian market is one of reasons for abuse. There is a trend seen that is women using these agents for skin lightening without any underling rashes or lesions without any prescription from dermatologist. There are no proper guidelines or updates regarding rational use of TCS and even dermatologists are unaware of future harm of these agents. Patient should be advised properly on its use, dosage, possible side effects before initiating therapy with agents. OTC drug use should be regulated with proper rules and regulations.
Acknowledgements
We would like to express sincere thanks to Department of Dermatology, The Karnataka Institute of Medical Science (KIMS), Hubli for providing necessary support and help. Also, would like to thanks to faculty members of Department of Pharmacy Practice, KLE College of pharmacy for their constant support and help.
References
- Al Dhafiri M, Alali AB, Alghanem ZA, Alsaleh ZW, Boushel EA, Alali ZB, et al. Topical steroid damaged face: A cross-sectional study from Saudi Arabia. Clin Pract. 2022; 12(1): 140-146.
[Crossref] [Google Scholar] [Pubmed]
- Kumar S, Goyal A, Gupta YK. Abuse of topical corticosteroids in India: Concerns and the way forward. J Pharmacol Pharmacother. 2016; 7(1): 1-5.
[Crossref] [Google Scholar] [Pubmed]
- Kakroo SN, Beg MA. Abuse of topical corticosteroids and its consequences: A prospective study. Int Arch Biomed Clin Res. 2018; 4(1): 182-185.
- Das A, Panda S. Use of topical corticosteroids in dermatology: An evidence-based approach. Indian J Dermatol. 2017; 62(3): 237.
[Crossref] [Google Scholar] [Pubmed]
- Jinagal J, Gupta PC, Pilania RK, Ram J. Systemic toxicity of topical corticosteroids. Indian J Ophthalmol. 2019; 67(4): 559-561.
[Crossref] [Google Scholar] [Pubmed]
- Hajar T, Leshem YA, Hanifin JM, Nedorost ST, Lio PA, Paller AS, et al. A systematic review of topical corticosteroid withdrawal (“steroid addiction”) in patients with atopic dermatitis and other dermatoses. J Am Acad Dermatol. 2015; 72(3): 541-549.
[Crossref] [Google Scholar] [Pubmed]
- Dhar S, Seth J, Parikh D. Systemic side-effects of topical corticosteroids. Indian J Dermatol. 2014; 59(5): 460.
[Crossref] [Google Scholar] [Pubmed]
- Rathi SK, D’Souza P. Rational and ethical use of topical corticosteroids based on safety and efficacy. Indian J Dermatol. 2012; 57(4): 251.
[Crossref] [Google Scholar] [Pubmed]
- Mehta AB, Nadkarni NJ, Patil SP, Godse KV, Gautam M, Agarwal S. Topical corticosteroids in dermatology. Indian J Dermatol Venereol Leprol. 2016; 82(4): 371-378.
[Crossref] [Google Scholar] [Pubmed]
- Murray E. Using topical corticosteroids safely and effectively. This Changed My Practice (UBC CPD). 2019.
- NIF. Topical corticosteroids. Northern Ireland Formulary. 2023.
- Mahar S, Mahajan K, Agarwal S, Kar HK, Bhattacharya SK. Topical corticosteroid misuse: The scenario in patients attending a tertiary care hospital in New Delhi. J Clin Diagn Res. 2016; 10(12): FC16-FC20.
[Crossref] [Google Scholar] [Pubmed]
- Dey VK. Misuse of topical corticosteroids: A clinical study of adverse effects. Indian Dermatol Online J. 2014; 5(4): 436.
[Crossref] [Google Scholar] [Pubmed]
- Su JC, Murashkin N, Wollenberg A, Svensson Å, Chernyshov P, Lio P, et al. Pharmacist recommendations regarding topical steroid use may contradict the standard of care in atopic dermatitis: An international, cross-sectional study. JAAD Int. 2021; 4: 13-14.
[Crossref] [Google Scholar] [Pubmed]
- Abraham MS, Sajeeth CI, Sreeja PA, Abraham BT. Prescribing pattern of corticosteroids and cost effective analysis of clobetasol and fluticasone for eczema in a Tertiary Care Teaching Hospital at Palakkad, Kerala. Int J Pharm Pharm Res. 2016; 6(3): 67-77.
- Lu H, Xiao T, Lu B, Dong D, Yu D, Wei H, et al. Facial corticosteroid addictive dermatitis in Guiyang City, China. Clin Exp Dermatol. 2010; 35(6): 618-621.
[Crossref] [Google Scholar] [Pubmed]
- Sinha A, Kar S, Yadav N, Madke B. Prevalence of topical steroid misuse among rural masses. Indian J Dermatol. 2016; 61(1): 119.
[Crossref] [Google Scholar] [Pubmed]
- Sheth NK, Nair PA. Topical steroids: Awareness and misuse among patients, pharmacists and general medical practitioner. Indian J Dermatol Venereol Leprol. 2021; 87(1): 54-59.
[Crossref] [Google Scholar] [Pubmed]
- Shumoukh SA, Shooq AA, Alya AA, Rasha SA, Halima ME. Misuse of topical corticosteroids in women in Hail region, Saudi Arabia. Int J Community Med Public Health. 2019; 6(5): 1880-1885.
Author Info
Jibin James1*, Ancy Chacko1, Nirmitha S Kumar2 and YM Angel Agnes22Department of Dermatology, Karnataka Institute of Medical Sciences (KIMS), Karnataka, India
Citation: James J: Topical Corticosteroids: A Review Article on its Adverse Effects and Abuse Leading to Local and Systemic Side Effects-Pharmacist Perspective
Received: 17-Aug-2023 Accepted: 11-Sep-2023 Published: 18-Sep-2023, DOI: 10.31858/0975-8453.14.9.587-590
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






