Research Article - (2023) Volume 14, Issue 1
Abstract
Objective: We assessed studies probing at vitamin D deficiencies in both positive and negative COVID-19 cases.
Methods: We measured mean, standard deviations, and 95% Confidence Interval (CI) of many studies to determine if there is a consistent relationship between vitamin D levels and COVID-19. Independent sample t-test compared non-survivors vs. survivors of COVID-19 and vitamin D levels, and moderate vs. severe COVID-19 symptoms and vitamin D levels.
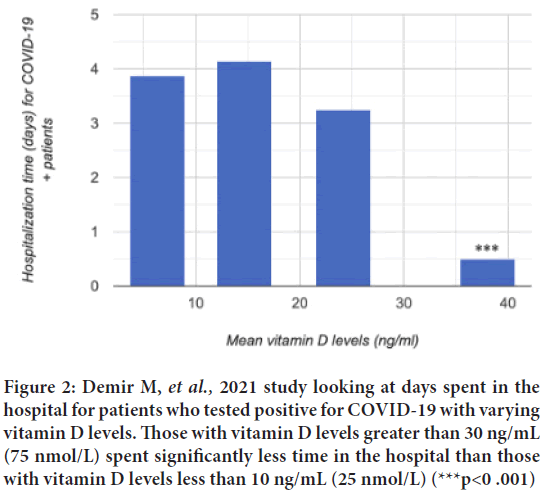
Results: We evaluated the difference in vitamin D levels (serum 25(OH)D, nmol/L) among those who tested positive for COVID-19 to those who tested negative. The average median serum 25(OH)D, nmol/L for patients who tested positive was 27.08 nmol/L (± 0.58 SD, 95% CI: 1.88) and the average median of serum 25(OH)D, nmol/L for patients who tested negative was 48.67 nmol/L (± 13.66 SD, 95% CI: 2.17) this difference was near significant (p=0.059). When looking at the relationship between vitamin D levels and severity of COVID-19 progression the result was not statistically significant, t(df)=0.84, p=0.216. When comparing the average values of vitamin D level among those who survived COVID-19 vs. those who did not the results were not statistically significant, t(269)=0.17, p=0.438.
Conclusion: There seems to be a correlation between vitamin D deficiency and likelihood of developing severe illness of COVID-19 when observing studies individually. However, when comparing studies on a larger scale it seems that the significant difference seems to fade.
Keywords
Vitamin D, COVID-19, serum 25-hydroxy vitamin D, severe illness
Introduction
COVID-19 is a respiratory disease first observed in 2019 that is caused by the novel SARS-CoV-2 virus. As of December 2021, the World Health Organization (WHO) reports that the impact of COVID-19 continues worldwide (WHO, 2021). According to the WHO, there have been roughly 282 million COVID-19 cases, and about 5.4 million reported deaths worldwide (WHO, 2021) (with many unaccounted for); COVID-19 continues to be a major area of concern and a significant health crisis (WHO, 2021). The virus can enter the body through air droplets by either the nose or mouth. The spikes on the outside of the virus capsule attached to the Angiotensin-Converting Enzyme-2 (ACE2) on nasal and bronchial epithelial cells. Once this interaction occurs, ACE2 is cleaved, and this allows for viral entry into the cells (WHO, 2021). Once rapid replication occurs, the inflammatory response can be triggered which can lead to increased coagulation, and disruption of the renin-angiotensin-aldosterone system leading to further tissue damage (WHO, 2021).
COVID-19 can trigger a heightened immune response, known as a cytokine storm. A cytokine storm can lead to hyper inflammation, and if not properly treated it can cause damage to tissues and organs in the body (Ruan Q, et al., 2020). A cytokine storm is initiated by the accumulation of many pro-inflammatory cytokines without enough anti-inflammatory cytokines to maintain a safe balance in the body. The reason why Vitamin D is such a vitamin of interest in respiratory illnesses is because it can decrease the production of pro-inflammatory cytokines, and increase the production of anti-inflammatory cytokines, causing a better balance in the body (Kumar R, et al., 2021). COVID-19 (SARS-CoV-2) can rapidly replicate in the lungs, and cause a cytokine storm, which can lead to Acute Respiratory Distress Syndrome (ARDS). ARDS can cause death, which is why finding ways to prevent the induction of a cytokine storm in patients is crucial to lowering the chances of severe disease by COVID-19 (Kumar R, et al., 2021).
There is interest in a possible relationship between vitamin D deficiency and development of COVID-19 because of prior studies linking vitamin D deficiency with other respiratory syndromes. In a meta-analysis looking at the effects of vitamin D supplementation and its effect on acute respiratory syndrome, Martineau et al. found that there was a significant reduction in the number of patients who experienced respiratory tract infections (Martineau AR, et al., 2017).
The way that Vitamin D helps to assist the immune system in fighting respiratory diseases is through the Vitamin D Receptor (VDR). It is through this pathway that cathelicidin is increased, an antimicrobial peptide in the body that has antiviral properties (Telcian AG, et al., 2017).
Vitamin D, in the form of calcitriol, can increase the production of macrophage cells, and inhibit the maturation of Antigen-Presenting Cells (APC), reducing the production of Interleukin (IL- 12), Tumor Necrosis Factor alpha (TNF-α), and Type 1 T helper (Th1) cells in the body (Cantorna MT, et al., 2008).
In a study looking at vitamin D deficiency and COVID-19 patient outcome, Radujkovic A, et al., found that patients deficient in vitamin D had significantly higher IL-6 levels possibly leading to a cytokine storm and therefore severe disease presentation (Radujkovic A, et al., 2020). This may point to an underlying relationship between low levels of vitamin D and increased severity in COVID-19 patients.
In this systematic review, we assessed studies that probed at vitamin D deficiencies in both positive and negative COVID-19 cases.
We compared vitamin D levels to see if there was a noticeable difference between the two groups; sufficient Vitamin D being serum 25(OH) D levels >30 ng/ml, insufficient serum 25(OH) D levels ranging from 21-29 ng/ ml, and deficient serum 25(OH) D levels as <20 ng/ml (Holick MF, 2009). Finally, through the review of several studies, we investigated whether more severe cases (measured via days in hospital and survival rates) of COVID-19 were correlated with low vitamin D levels.
Materials and Methods
We used PubMed to find research articles examining the relationship between Vitamin D and COVID-19. We were able to narrow our search by looking for articles that focused on the difference between vitamin D levels in positive and negative COVID-19 patients. We also explored articles that measured the difference in severity progression of COVID-19 in relation to their vitamin D levels. From this collection of 19 articles in April of 2021, we were able to further eliminate articles based on what they observed in their study. We eliminated studies that did not look at any of the following: Comparing median Serum 25(OH)D (nmol/L, or ng/ml) level control vs.median Serum 25(OH)D (nmol/L, or ng/ml) level+COVID-19, Hospital stay (days) vs. mean Serum 25(OH)D (nmol/L, or ng/ml) levels, median or mean Serum 25(OH)D (nmol/L, or ng/ml) levels in comparison between those who survived vs.non-survivors, and Severity in COVID-19 symptoms and Serum 25(OH)D (nmol/L, or ng/ml) levels. We eliminated studies that were systematic reviews or meta-analyses. We included retrospective cohort studies, cross-sectional studies, prospective cohort studies, case control studies, observational cohort studies, and one clinical study. A second search for studies was conducted in June 2021. Articles were found via PubMed and Clinical Key. Each article was reviewed for the same objectives and with the same criteria as in April, 2021. Following the search, in both April and June, 133 articles were found that related to our objectives and criteria, and a total of 19 articles were used for data collection.
The mean and standard deviations of the vitamin D levels in patients who tested positive and negative for COVID-19 were analyzed. We used Practical Meta-Analysis Effect Size Calculator developed by David B Wilson, Ph.D., George Mason University (https://www.campbellcollaboration.org/escalc/html/EffectSizeCalculator-OR2.php) when looking at COVID-19 status and vitamin D (n=50-80 nmol/L) deficient levels. In this systematic review, we measured mean, standard error and P-value for three studies looking at vitamin D levels in positive vs. negative COVID-19 patients. We calculated the means, standard deviations, and 95% Confidence Interval (CI). We also used a t-test calculator for two independent means (https://www.socscistatistics.com/tests/studentttest/default.aspx) to determine if there is a difference in vitamin D levels between moderate vs. severe COVID-19 symptoms and a difference in vitamin D levels between survivors and non-survivors of COVID-19. Finally, we qualitatively observed seven studies that observed vitamin D levels and length of stay in the hospital (days).
Results
Three studies carried out by Baktash V, et al., 2021, D’Avolio A, et al., 2020, and Luo X, et al., 2021 were analyzed to compare the difference in vitamin D (25(OH)D, nmol/L) levels among those who tested positive for COVID-19 (n=432) to those who tested negative (n=675). The mean and standard deviations of the vitamin D levels in patients who tested positive and negative for COVID-19 were analyzed. We used the previously discussed meta-analysis effect size calculator when examining COVID-19 status and vitamin D (normal=50-80 nmol/L) deficient levels (Hollis BW, 2005). In this descriptive review, we measured mean, standard deviations, and 95% CI, and t-values of 19 studies to determine if there is a consistent relationship between vitamin D levels and COVID-19.
It was found that the average median serum 25(OH)D for patients who tested positive was 27.08 nmol/L (10.83 ng/mL) (± 0.58 SD, 95% CI: 1.88) and 48.67 nmol/L (19.47 ng/mL)(± 13.66 SD, 95% CI: 2.17) for patients who tested negative. The mean vitamin D levels, the standard error, and p-value were calculated via Excel; this difference was near significant (p=0.059) as seen in Figure 1.
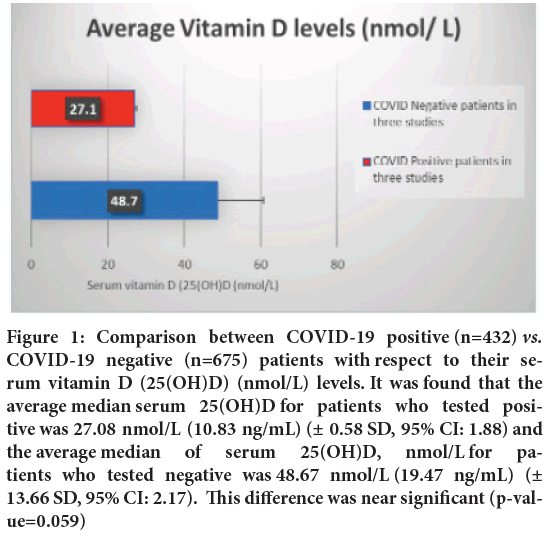
Figure 1: Comparison between COVID-19 positive (n=432) vs. COVID-19 negative (n=675) patients with respect to their serum vitamin D (25(OH)D) (nmol/L) levels. It was found that the average median serum 25(OH)D for patients who tested positive was 27.08 nmol/L (10.83 ng/mL) (± 0.58 SD, 95% CI: 1.88) and the average median of serum 25(OH)D, nmol/L for patients who tested negative was 48.67 nmol/L (19.47 ng/mL) (± 13.66 SD, 95% CI: 2.17). This difference was near significant (p-value=0.059)
When looking at the effects of vitamin D on inflammation levels, Radujkovic A, et al., found that IL-6 levels were significantly higher in vitamin D deficient patients, than in patients with normal levels of vitamin D (Radujkovic A, et al., 2020). It was also found that patients with vitamin D levels above 75 nmol/L had significantly lower levels of C-Reactive Protein (CRP), an indicator of inflammation, compared to those with vitamin D levels below 75 nmol/L. However, other studies found no significant difference in the CRP levels associated with vitamin D levels. Lastly, in patients with vitamin D levels <30 nmol/L survival probability of COVID-19 decreased significantly, compared to those whose vitamin D levels were >30 nmol/L.
In patients with various ranges of vitamin D levels, Demir M, et al., 2021 found that patients with vitamin D levels above 30 ng/mL had significantly lower levels of CRP, an indicator of inflammation, than those with vitamin D levels below 30 ng/mL. However, CRP levels showed no significant difference associated with vitamin D levels in a study by Baktash V, et al., 2021. Lastly, in a study comparing severity of COVID-19 and vitamin D levels, their inpatient subgroup (presentation of severe disease) had lower vitamin D levels as compared to the outpatient subgroup (presentation of less severe disease). This difference was found to be statistically significant with a p value of 0.004 (Radujkovic A, et al., 2020).
The most consistent measurement among various studies, for severity of disease progression in patients who tested positive for COVID-19 with varying vitamin D levels, was days spent in the hospital. The Demir M, et al., 2021 study found that those with vitamin D levels greater than 30 ng/mL (75 nmol/L) spent significantly less time in the hospital than those with vitamin D levels less than 10 ng/mL (25 nmol/L) (***p<0.001) as seen in Figure 2. Other studies found a similar outcome. When looking at the number of days spent in the hospital in a study by Luo X, et al., 2021 they discovered that the median number of the days spent in the hospital were fewer in those whose serum vitamin D levels were higher, but these differences were not statistically significant. Osman W, et al., 2021 found that there was no significant difference between the hospital days and vitamin D level range. Similarly, Maghbooli Z, et al., 2020 found that there was no notable difference as well. On the contrary, Vassiliou AG, et al., 2020 and Orchard L, et al., 2021 demonstrated in their data that those with higher levels of vitamin D levels stayed in the hospital longer than those whose vitamin D levels were lower. Additionally, Szeto B, et al., 2021 also found that patients with vitamin D levels >20 ng/ml stayed in the hospital on average longer than those who had vitamin D levels <20 ng/ml.
Figure 2: Demir M, et al., 2021 study looking at days spent in the hospital for patients who tested positive for COVID-19 with varying vitamin D levels. Those with vitamin D levels greater than 30 ng/mL (75 nmol/L) spent significantly less time in the hospital than those with vitamin D levels less than 10 ng/mL (25 nmol/L) (***p<0 .001)
When comparing moderate vs.severe COVID-19 symptomatic patients (Table 1), we were able to compare four studies (de Smet D, et al., 2021; Ahmed S and Jafri L, 2020; Ye K, et al., 2021; Luo X, et al., 2021). We utilized calculator.net to calculate the mean of the medians and the standard deviation with a 95% confidence interval level when looking at the relationship between vitamin D levels and severity of COVID-19 progression. With a total number of 537 patients, the mean of the median vitamin D levels of 364 patients, across all three studies, who were categorized to have moderate COVID-19 symptoms, was 45.025 nmol/L ± 10.531 as compared to 173 patients with severe COVID-19 symptoms having a mean of the median vitamin D levels of 38.075 nmol/L ± 9.241 (Luo X, et al., 2021; de Smet D, et al., 2021; Ahmed S and Jafri L, 2020; Ye K, et al., 2021). An independent sample t-test was computed to compare the average values of these two groups using a t-test calculator, on the Social Science Statistics website, for two independent means. The result was not statistically significant, t(df)=0.84, p=0.216, indicating no differences between the moderate and severe symptom groups concerning level of vitamin D.
| Study | Definition |
|---|---|
| Luo X | Mild: Symptoms with no signs of pneumonia on imaging |
| Moderate: Fever, respiratory symptoms with radiological evidence of pneumonia | |
| Severe: Respiratory distress, respiratory rate ≥ 30 breaths/min, hypoxemia, oxygen saturation (SpO2) ≤ 93% (at rest), or lung infiltrates of >50% within 24-48 h | |
| Critical: Respiratory failure requiring mechanical ventilation, shock, or multiple organ dysfunction requiring intensive care unit monitoring and treatment. | |
| Jain A | Severe: Requiring admission to Intensive Care Unit (ICU). |
| Karahan S | Mild: Mild clinical symptoms and normal lung on radiologic imaging. |
| Moderate: Fever and pulmonary symptoms along with pneumonia on radiologic imaging. | |
| Severe: Respiratory distress (≥ 30 breaths/min); oxygen saturation ≤ 93% at rest; or PaO2/FiO2 ≤ 300 mmHg or chest imaging shows obvious lesion progression >50% within 24-48 hours | |
| Critical: Respiratory failure and need for mechanical ventilation, shock, or other organ failures that requires ICU care | |
| Pizzini A | Mild: Patients in outward treatment |
| Moderate: Patients in inward treatment | |
| Severe: Patients requiring oxygen supplementation |
Table 1: Definition of COVID-19 severity by study
We looked at three studies, Luo X, et al., 2021; de Smet D, et al., 2021; Ahmed S and Jafri L, 2020 that measured vitamin D levels in survivors vs. non-survivors of COVID-19. To compare these data, we utilized calculator. net to calculate the mean of the medians and the standard deviation with a 95% confidence interval level to get an average vitamin D level among those who survived COVID-19 vs.those who did not. With a total of 271 patients, 35 who died, and 236 who survived, the mean vitamin D level of COVID-19 survivors was 15.43 ng/ml with a SD of ± 4.932, and the mean vitamin D levels of those who were non-survivors of COVID-19 was 14.60 ng/ml with a SD of ± 6.311 (Luo X, et al., 2021; de Smet D, et al., 2021; Ahmed S and Jafri L, 2020). When comparing the average values of these two groups, an independent sample t-test was computed to compare the average values of these two groups using a t-test calculator, on the Social Science Statistics website, for two independent means. The results were not statistically significant, t(269)=0.17, p=0.438, indicating no differences between the survivor and non-survivor groups concerning vitamin D levels.
Discussion
While it seems, when observing individual studies, that there is a substantial relationship between COVID-19 positivity, symptom progression and vitamin D levels, it cannot be concluded from the studies included in this review that there is any statistical significance. When looking at the data and comparing studies to one another on a larger scale, these individual significant findings seem to wane. The primary reasons seem to lie in the lack of uniformity in parameters and statistical analysis of the vitamin D levels and deficiency, as well as COVID-19 positivity rates and severity (Table 1).
Studies by Baktash V, et al., 2021, D’Avolio A, et al., 2020, and Luo X, et al., 2021 were analyzed to compare the difference in vitamin D (25(OH)D, nmol/L) levels among those who tested positive for COVID-19 (n=432) to those who tested negative (n=675) and there was a near significance, when comparing the means. However, if more studies were able to be compared, this finding might change.
When looking at the effects of CRP levels (measurement of inflammation) among three studies: Radujkovic A, et al., 2020; Demir M, et al., 2021 and Baktash V, et al., 2021 the data from these studies are conflicting. Baktash looked at CRP levels in the context of comparing vitamin D levels <12 ng/ mL as compared to vitamin D levels >12 ng/mL, and found no significance (Baktash V, et al., 2021). However, when reporting the median instead of the mean, the Demir study found that vitamin D levels <12 ng/mL, as compared to the outpatient subgroup (presentation of less severe disease) whose vitamin D levels were >12 ng/mL were significantly different (Demir M, et al., 2021). The difference in reporting mean vs.median made it difficult to compare and conclude that Vitamin D has a meaningful effect on CRP levels. When Radujkovic et al. reports that vitamin D levels above 75 nmol/L had significantly lower levels of C-Reactive Protein (CRP), it cannot be compared to those that measured effects of vitamin D levels at much lower levels. More studies of measuring CRP levels at vitamin D levels above 75 nmol/L have to be considered before making a definite statement one way or the other, as other studies with various vitamin D levels and measurements produce differing results.
Severity of COVID-19 based on days spent in hospital is inconclusive. Two studies by Demir M, et al., and Luo X, et al., report that increased vitamin D levels are correlated with fewer days in the hospital. However, two studies by Osman W, et al., 2021 and Maghbooli Z, et al., 2020 report that there is no difference in hospital stay between those with higher vs.lower vitamin D levels. Finally, three studies, Vassiliou AG, et al., 2020, Orchard L, et al., 2021 and Szeto B, et al., 2021 report the opposite, that those with higher vitamin D levels were associated with more days in hospital.
When comparing the vitamin D levels of non-survivors vs. survivors of COVID-19, on average they differed slightly; survivors on average had a higher vitamin D level than those who passed; however, it was not significant. Additionally, when comparing the average median vitamin D levels of moderate vs.severe COVID-19 disease presentation, this data proved the difference to be insignificant. Therefore, we need more data and studies that use the same measurements and statistical methods to observe the relationship more clearly.
Conclusion
COVID-19 has had a horrendous effect on the world, mostly from the threat of death, initial lack of data, and possible long term effects of the disease. Finding ways to lessen the progression of the disease is paramount, and vitamin D is a readily available supplement that could make a great impact if proven that it could statistically prevent or lessen the severity of COVID-19.
In this systematic review, we assessed studies that probed at vitamin D deficiencies in both positive and negative COVID-19 cases, and investigated whether more severe cases of COVID-19 were correlated with low vitamin D levels. While we found in many studies that vitamin D deficiency demonstrated a significant difference in those that were positive vs. negative for COVID-19, as well as a significant difference in the days spent in the hospitals after contracting COVID-19, when comparing studies on a larger scale it seems that the significant difference seems to fade. In this review we found that the difference between vitamin D levels and positivity rates for COVID-19 were nearly significant in collective comparison. We compared days in the hospital and vitamin D levels, and the data was inconsistent. While survivors vs. non-survivors had on average higher vitamin D levels, it is not determined that these were significant findings.
Due to the lack of consistent measurements and statistical analysis in the published literature, it was difficult to gather a large number of studies. For some studies, authors used the mean as a way to compare groups, while others used median to do so. Some studies focused on a younger population, while others focused on an older one, this led to many difficulties with comparison on a large scale. Lastly, studies varied in their vitamin D cut-off levels, making it harder to compare vitamin D efficacy levels.
From this review it is clear that vitamin D does play a role in the immune response in COVID-19 and that taking a vitamin D supplement may be warranted if one is deficient in vitamin D. Gathering more studies that have uniform parameters to observe the relationship between COVID-19 and vitamin D would be beneficial, because further research and more data would help to decipher if there is a consistent relationship, and beneficial effects of preventing severe COVID-19 disease progression.
Declarations
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
The authors confirm contribution to the paper as follows: study conception and design, data collection, analysis and interpretation of results, and draft manuscript preparation: L Kersh. All authors reviewed the results and approved the final version of the manuscript.
Acknowledgements
We thank Michael B. Roberts, PsyD Director of Institutional Research at PCOM for his helpful statistical advice and Kyla Geary, a Research Assistant III at the Philadelphia College of Osteopathic Medicine (PCOM), for her editorial guidance.
References
- WHO. COVID-19 responsible for at least 3 million excess deaths in 2020. World Health Organization. 2021.
- WHO. WHO Coronavirus (COVID-19) Dashboard. World Health Organization. 2021.
- WHO. COVID-19 (Novel Coronavirus). World Health Organization. 2021.
- Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020; 46(5): 846-848.
[Crossref] [Google Scholar] [Pubmed]
- Kumar R, Rathi H, Haq A, Wimalawansa SJ, Sharma A. Putative roles of vitamin D in modulating immune response and immunopathology associated with COVID-19. Virus Res. 2021; 292: 198235.
[Crossref] [Google Scholar] [Pubmed]
- Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ. 2017; 356: 6583.
[Crossref] [Google Scholar] [Pubmed]
- Telcian AG, Zdrenghea MT, Edwards MR, Laza-Stanca V, Mallia P, Johnston SL, et al. Vitamin D increases the antiviral activity of bronchial epithelial cells in vitro. Antiviral Res. 2017; 137: 93-101.
[Crossref] [Google Scholar] [Pubmed]
- Cantorna MT, Yu S, Bruce D. The paradoxical effects of vitamin D on type 1 mediated immunity. Mol Aspects Med. 2008; 29(6): 369-375.
[Crossref] [Google Scholar] [Pubmed]
- Radujkovic A, Hippchen T, Tiwari-Heckler S, Dreher S, Boxberger M, Merle U. Vitamin D deficiency and outcome of COVID-19 patients. Nutrients. 2020; 12(9): 2757.
[Crossref] [Google Scholar] [Pubmed]
- Holick MF. Vitamin D status: Measurement, interpretation, and clinical application. Ann Epidemiol. 2009; 19(2): 73-78.
[Crossref] [Google Scholar] [Pubmed]
- Baktash V, Hosack T, Patel N, Shah S, Kandiah P, van den Abbeele K, et al. Vitamin D status and outcomes for hospitalised older patients with COVID-19. Postgrad Med J. 2021; 97(1149): 442-447.
[Crossref] [Google Scholar] [Pubmed]
- D’Avolio A, Avataneo V, Manca A, Cusato J, de Nicolò A, Lucchini R, et al. 25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2. Nutrients. 2020; 12(5): 1359.
[Crossref] [Google Scholar] [Pubmed]
- Luo X, Liao Q, Shen Y, Li H, Cheng L. Vitamin D deficiency is associated with COVID-19 incidence and disease severity in Chinese people. J Nutr. 2021; 151(1): 98-103.
[Crossref] [Google Scholar] [Pubmed]
- Hollis BW. Circulating 25-hydroxyvitamin D levels indicative of vitamin D sufficiency: Implications for establishing a new effective dietary intake recommendation for vitamin D. J Nutr. 2005; 135(2): 317-322.
[Crossref] [Google Scholar] [Pubmed]
- Demir M, Demir F, Aygun H. Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease. J Med Virol. 2021; 93(5): 2992-2999.
[Crossref] [Google Scholar] [Pubmed]
- Osman W, al Fahdi F, al Salmi I, al Khalili H, Gokhale A, Khamis F. Serum Calcium and Vitamin D levels: Correlation with severity of COVID-19 in hospitalized patients in Royal Hospital, Oman. Int J Infect Dis. 2021; 107: 153-163.
[Crossref] [Google Scholar] [Pubmed]
- Maghbooli Z, Sahraian MA, Ebrahimi M, Pazoki M, Kafan S, Tabriz HM, et al. Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection. PloS One. 2020; 15(9): e0239799.
[Crossref] [Google Scholar] [Pubmed]
- Vassiliou AG, Jahaj E, Pratikaki M, Orfanos SE, Dimopoulou I, Kotanidou A. Low 25-hydroxyvitamin D levels on admission to the intensive care unit may predispose COVID-19 pneumonia patients to a higher 28-day mortality risk: A pilot study on a Greek ICU cohort. Nutrients. 2020; 12(12): 3773.
[Crossref] [Google Scholar] [Pubmed]
- Orchard L, Baldry M, Nasim-Mohi M, Monck C, Saeed K, Grocott MP, et al. Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients. Clin Chem Lab Med. 2021; 59(6): 1155-1163.
[Crossref] [Google Scholar] [Pubmed]
- Szeto B, Zucker JE, la Sota ED, Rubin MR, Walker MD, Yin MT, et al. Vitamin D status and COVID-19 clinical outcomes in hospitalized patients. Endocr Res. 2021; 46(2): 66-73.
[Crossref] [Google Scholar] [Pubmed]
- de Smet D, de Smet K, Herroelen P, Gryspeerdt S, Martens GA. Serum 25 (OH) D level on hospital admission associated with COVID-19 stage and mortality. Am J Clin Pathol. 2021; 155(3): 381-388.
[Crossref] [Google Scholar] [Pubmed]
- Ahmed S, Jafri L. Prognostic Utility of Baseline 25-Hydroxy Vitamin D Levels in Hospitalised COVID-19 Patients: Hope or Hype?. J Coll Physicians Surg Pak. 2020; 30(10): 183-184.
[Crossref] [Google Scholar] [Pubmed]
- Ye K, Tang F, Liao X, Shaw BA, Deng M, Huang G, et al. Does serum vitamin D level affect COVID-19 infection and its severity?-A case-control study. J Am Coll Nutr. 2021; 40(8): 724-731.
[Crossref] [Google Scholar] [Pubmed]
Author Info
Lydia Maria Kersh1*, Kyla Geary2, Michael B Roberts2 and Farzaneh Daghigh32Department of Institutional Research, Philadelphia College of Osteopathic Medicine, Philadelphia, United States
3Department of Biomedical Sciences, Philadelphia College of Osteopathic Medicine, Philadelphia, United States
Citation: Kersh LM: What is the Impact of Vitamin D Levels on COVID-19 Severity?: A Systematic Review
Received: 02-Dec-2022 Accepted: 27-Dec-2022 Published: 03-Jan-2023, DOI: 10.31858/0975-8453.14.1.47-51
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ARTICLE TOOLS
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3